Novel ‘assessment center’ will be a partner in care by serving as an engine of structured data collection
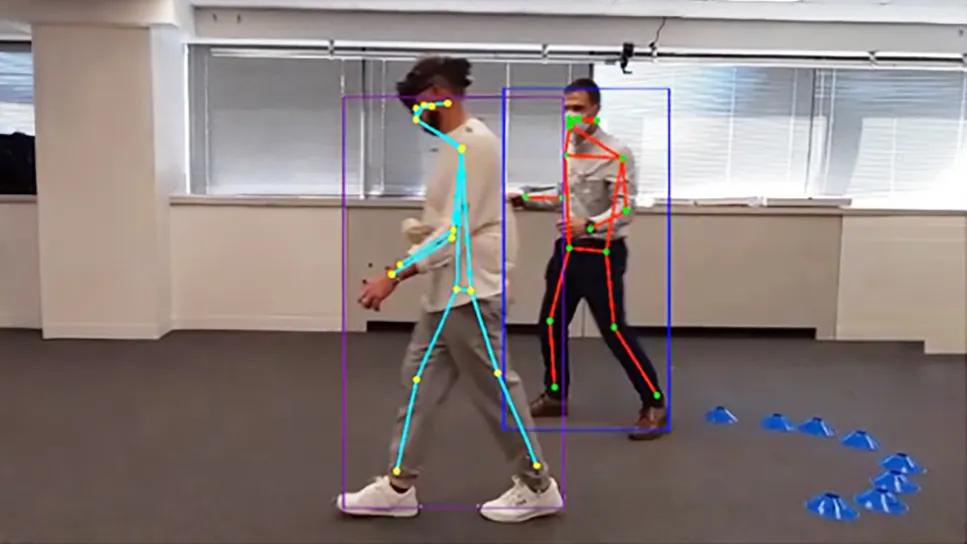
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/93e650e8-f7ae-4c9b-a2fe-92ab4db6b59c/neuro-building-design-update)
person walking with a stick-figure overlay on his body
As reported in a recent companion article, construction of the physical frame of Cleveland Clinic’s forthcoming 1 million-square-foot Neurological Institute building was completed earlier this year. When the facility opens for patient care on the health system’s Main Campus in early 2027, it will house 210 inpatient rooms (to be expanded to 300), 120 outpatient exam rooms, 36 neurological ICU beds and 14 operating rooms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“This will be the largest and most technologically advanced neuroscience-focused facility in the world,” says Cleveland Clinic Neurological Institute Chief Andre Machado, MD, PhD. “We believe its integration of clinical care with research and education will attract the finest neuroscience talent to serve at Cleveland Clinic.”
The building will be equipped throughout with state-of-the-art technology intended to put Cleveland Clinic at the forefront of what Neurological Institute leaders call the “3 D’s” — digitization, discovery and distance health — in service of exceptional neurological care through data-driven decision making. This article profiles how two of those D’s — digitization and discovery — fundamentally inform a centerpiece of the new building known as the assessment center.
“We are designing this building to be a partner in patient care by playing a key part in data collection,” says neurologist Robert Bermel, MD, Director of the Mellen Center for Multiple Sclerosis Treatment and Research. “Much of the neurological exam will be completed while patients walk from the entrance and make their way to their physician’s office for their appointment.”
This characterization of neurological function will take place largely in the assessment center, a centralized space on the ground floor where patients will check in digitally and then efficiently complete a series of neuroperformance modules designed to assess a specific neurological function or group of functions.
Patients will first encounter the gait and balance module as they walk down a hallway equipped with sensors and cameras connected to software developed at Cleveland Clinic that will automatically characterize the quality of patients’ gait. Stride length, gait speed and symmetry, arm swing, posture and other characteristics will be captured. “The patient walks naturally through the digitization pathway, and we can collect quantitative and qualitative measures of their gait,” Dr. Bermel explains.
Advertisement
“Gait speed and other measures of mobility have been proposed as the ‘sixth vital sign’ for decades,” adds Jay Alberts, PhD, Vice Chair of Innovation in the Neurological Institute, who has been deeply involved in the design and development of the assessment center’s gait and balance module. “This will be the first example of gathering this vital information as part of routine clinical practice. The collected data are anything but routine, as they will provide unprecedented insight into disease progression and treatment effectiveness while also enhancing disease diagnostics.”

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/ffae602a-336b-4a09-ab11-f1ff4cd365f1/neuro-building-design-new-update-inset-1)
Rendering of the hallway for the gait and balance module.
Patients next complete the complex figure drawing module, in which they interact with a touch screen to copy a complex figure illustration. Using artificial intelligence, a computer linked to the screen provides immediate assessments of visuospatial function, cognition and upper extremity function.
Next comes the voice pattern analysis module, in which the patient is asked to describe in one minute a picture displayed on a screen. The patient’s voice is recorded, yielding assessments of speech pattern, cadence, presence or absence of tremor, and other measures that can signal neurodegeneration. The content of the description is also assessed, yielding cognitive measures related to how completely and accurately the patient is able to describe the picture.
“The assessment center’s modules were designed to be efficient and almost game-like, to maximize the yield of neurological data while reducing the chance for patient frustration,” Dr. Bermel notes.
Advertisement
At computer stations where patients take the drawing and voice assessments, they also can self-measure vital signs such as blood pressure and pulse. “The assessment center will operate as a self-directed process for patients who are capable of that, with assistance provided as needed,” Dr. Bermel says. “The idea is to automatically take care of as much data collection as we can ahead of the visit to make the visit with the provider as rich as possible, freeing up time to discuss with the patient all the data we’ve collected over time and customize a treatment plan.”
The rationale for the assessment center is to collect high-quality objective data that reflect how patients are functioning in the real world. Integration of all these data into the electronic health record will allow providers to better educate patients and collaboratively monitor their condition. “Gathering a set of meaningful data in a standardized manner over time will advance our understanding of neurological disease and further the practice of precision medicine for all neurological patients,” Dr. Alberts observes, noting that traditional clinical scales for neurological diseases are often not relatable or familiar to patients.
“In contrast,” he continues, “we have patients say that when providers review their own data with them, they feel like they are on the same page in discussing their disease and the potential effects of various medications or interventions.”
“The weakest link in terms of data quality is often information on how a patient is functioning in the real world as they live with their disease,” Dr. Bermel adds. “This space is an opportunity to overcome that limitation and efficiently capture meaningful, objective data to characterize how patients are doing. Data collection over multiple visits will give us a longitudinal picture.”
Advertisement
Balancing the need for data with the need to maintain patient privacy, measures such as automatic face blurring are applied to video assessments and video is analyzed using the same standards of privacy with which Cleveland Clinic protects all health data.
“We will be transparent about data collection,” Dr. Bermel says. “Based on our experience in the Mellen Center for Multiple Sclerosis and Cleveland Clinic’s Center for Neurological Restoration, there is enthusiasm among most patients to complete these types of assessments as they inform the most personalized treatment for themselves and contribute to broader research efforts to better understand and treat a neurologic disease that will affect others. We already see this from conversations with patients, most of whom encourage us to put research data and biospecimens to use against the common enemy, which is neurologic disease.”
Meanwhile, the technology proposed for the assessment center has undergone technical validation testing via a prototype system in Cleveland Clinic’s Mellen Center building. That testing was successfully completed in October 2024, demonstrating good technical operation to support the needed throughput and archiving of data for research. A six-month clinical validation study is expected to begin soon, with the aim of quantifying the assessment center’s novel measures and relating them to current best-practice neurological measures.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/6294a058-7280-41e8-a993-96b4527377fb/neuro-building-design-new-update)
Photo from a validation testing session for the gait and balance module showing data outputs from the markerless motion capture assessment.
“The technologies we are planning are an extension and enhancement of more basic computer tablet-based modules for testing core neurologic functions that Cleveland Clinic has been using at scale in the ‘waiting room of the future’ in our Mellen Center and Center for Neurological Restoration for several years now,” notes Dr. Bermel. “Preliminary data and feasibility of this approach have been well established, as we have reported in the literature (Neurol Clin Pract. 2020;10[3]:222-231), so we feel well positioned to innovate further in this space.”
Advertisement
The new building’s extensive data-collection capabilities promise important benefits in research as well, raising the second of the 3 D’s behind its mission: discovery. The structured data captured at every visit will be available not only for real-time care of the individual patient but also for use — in anonymized form — by researchers in aggregate. The data will be leveraged to monitor care quality and treatment efficacy. More broadly, data will be analyzed longitudinally and in aggregate to identify trends and patterns to inform research questions and help guide development of treatments of the future.
“Data from the hundreds of thousands of patient encounters in this building each year will collectively yield a powerful database that can be examined in many ways for insights that may lead to cures,” Dr. Bermel says. “This will expand how patients can be engaged in clinical research. No longer will they need to be part of a randomized clinical trial to contribute to neurological discoveries.”
Moreover, clinical data collected in the building will complement findings from the ongoing Cleveland Clinic Brain Study, a landmark longitudinal investigation of thousands of adult volunteers with no known neurological disease that’s designed to identify biomarkers of neurological disorders before symptoms manifest. “The types of data collected in the assessment center will be similar to data collected in our Brain Study,” notes Dr. Machado, one of the Brain Study’s co-principal investigators. “Taken together, these data will provide a picture of findings across the entire spectrum of neurological disease, from neurologically healthy and presymptomatic individuals in the Brain Study to patients in early to advanced stages of neurological disease being treated in our new building.”
A prime example is voice pattern analysis, which is being assessed in the Brain Study as well as in the assessment center. Once a voice signature of a condition like Parkinson’s disease (PD) can be identified in patients with a verified PD diagnosis, clinician scientists can work to identify the earliest versions of that voice signature in the Brain Study data and potentially use the insights to diagnose PD at an earlier stage.
“These combined efforts represent an unprecedented opportunity to characterize the full continuum of neurological disease,” Dr. Machado concludes.
Advertisement
Today’s research helps illuminate tomorrow’s needs
What it’s like working in neurology critical care and what to consider before entering the specialty
Case series links catastrophic outcomes to therapy initiation within 48 hours post-procedure
Scientific program chair reflects on what may resonate longest from this year’s neurosurgery conference
Input from these central stakeholders is leading us to design for healing and hope
Subtle information gleaned from clinical examinations prompted concern
Neurology is especially well positioned for opportunities to enhance clinical care and medical training
How functional restoration can help children with these conditions marked by unexplained pain with stigmatized symptoms