Biomarkers urgently needed
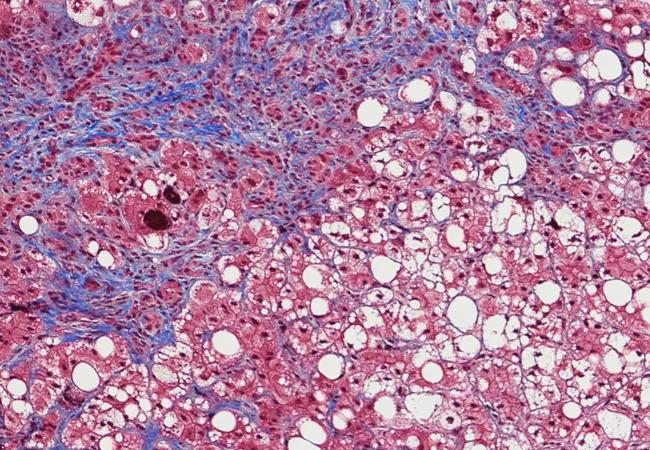
Nonalcoholic fatty liver disease (NAFLD) affects up to 75 percent of patients with type 2 diabetes. Patients with these two intertwined diseases can have an increased likelihood of developing both diabetic complications and the most severe NAFLD outcomes such as advanced fibrosis also known as cirrhosis.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Researchers have struggled, though, to find reliable biomarkers for predicting advanced fibrosis in diabetics and must rely on costly imaging tests and liver biopsy.
Recently, Cleveland Clinic investigators performed a retrospective chart analysis to determine the validity of different non-invasive fibrosis scores — the Fibrosis 4 score, the AST to platelet ration index (APRI) and the NAFLD fibrosis score (NFS) — that are commonly used to determine advanced fibrosis in hepatitis C and NAFLD patients would also work for type-2 diabetic patients.
“We’ve looked at 1,145 patients with a diagnosis of type 2 diabetes who had liver biopsy for suspected nonalcoholic fatty liver disease and, using noninvasive scores, we calculated how many should have advanced fibrosis and compared them to the biopsy results,” says Amandeep Singh, MD, clinical nutrition fellow, one of the authors on the study which was recently published in August in Clinical Gastroenterology. Dr. Singh presented his study at the WCOG at ACG2017.
The mean age of the study participants was 54, 60 percent were women and 94 percent were Caucasian. Ninety one percent of the study population was above normal weight limit. Sixty percent had hyperlipidemia and 22 percent had CKD, 42 percent were on insulin therapy and 48 percent were on anti-lipid agents. Liver biopsy showed 31.7 percent had advanced fibrosis (stage 3 and 4).
Dr. Singh and colleagues calculated both sensitivity and specificity and area under the ROC curve to predict the overall accuracy of each score. In general, they found that the scores had greater specificity than sensitivity when it came to predicting advanced fibrosis:
Advertisement
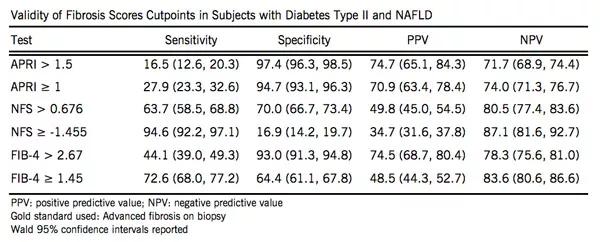
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e8e56d4e-4e68-4976-a412-b02774567f41/17-DDI-3953-Validity-CQD-Inset-1_jpg)
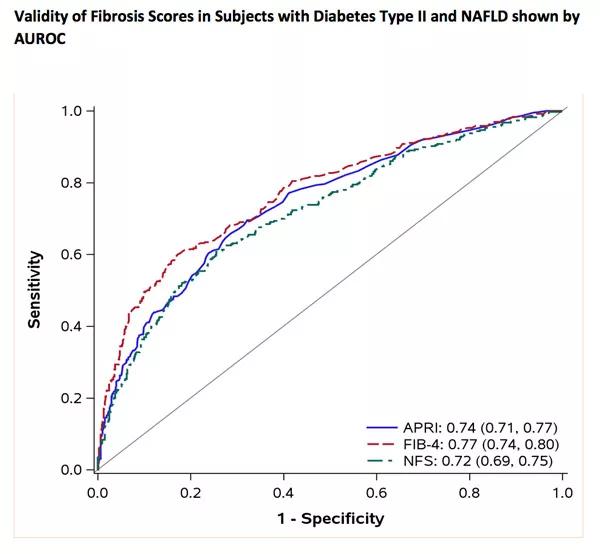
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/695c7860-25a1-476b-983f-533bff92d7c3/17-DDI-3953-Validity-CQD-Inset-2_jpg)
The results show that providers who use these scores especially FIB-4 and APRI, can rule in advanced fibrosis in patients but they may also miss patients with advanced fibrosis due to lack of sensitivity.
Dr. Singh says using such scores – while not perfect – gives doctors a way to start to narrow down patients at risk. Primary care doctors in particular need to consider using them when evaluating type 2 diabetics, he adds says. “Because a lot of people rely just on the labs and if you look at basic liver function tests, most of the time they are normal so they fool you. Normal labs don’t mean there isn’t a liver abnormality.
“We urgently need a test with high sensitivity and specificity to screen diabetic patients with suspected fatty liver disease and act before the advance disease set in and it’s too late.”
Advertisement
Advertisement

Benefits of neoadjuvant immunotherapy reflect emerging standard of care

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Potentially cost-effective addition to standard GERD management in post-transplant patients

Findings could help clinicians make more informed decisions about medication recommendations

Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care

Retrospective analysis looks at data from more than 5000 patients across 40 years