Study leverages data from the ROSETTA trial
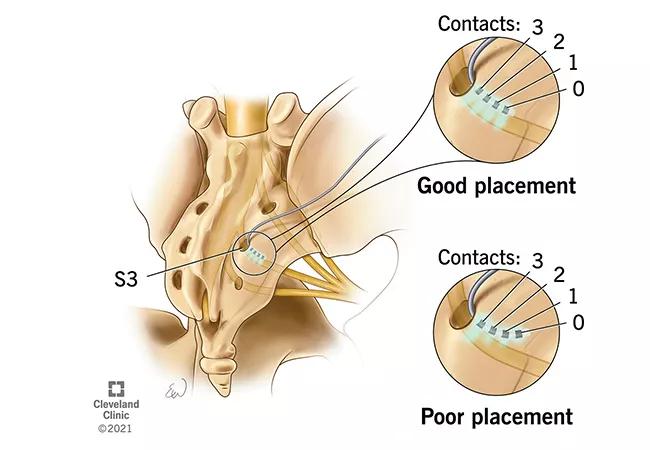
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/3440df9c-27dd-4d82-8347-328651d25f86/23-URL-4086314-CQD-650x450-1_jpg)
sacral neuromodulation lead
Findings from a study investigating intraoperative sacral neuromodulation (SNM) lead placement identifies factors associated with successful outcomes in patients with overactive bladder (OAB) who received the treatment. The study, published in The Journal of Urology, was featured as the journal’s cover story in August 2023.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Though SNM, a third-line therapy for patients with refractory OAB, has been around for several decades, little is known about what determines whether a patient will respond to treatment.
Urologist Bradley Gill, MD, first author of the study, remarks it’s one of the rare treatments where a patient gets to ‘try before they buy,’ so to speak. “There’s a test period where wires are inserted through the skin to the nerves, and patient can return home with an external battery pack. They are basically able to try it out for a couple of weeks to see if it works,” he says. If it’s successful, the patient will return for permanent implantation.
“Over time, there have been a number of smaller, single-institution studies where groups would look at their retrospective databases and try to tease out what predicted whether or not a patient would respond to the treatment, but the data have been relatively inconclusive.”
This led Dr. Gill and colleagues to develop a sub-study within the ROSETTA trial, a prospective, multicenter investigation comparing OBTX-A and SNM in women with refractory OAB.
Dr. Gill, who was a medical student at Cleveland Clinic Lerner College of Medicine with a background in biomedical engineering when the ROSETTA study was enrolling patients, recalls a conversation he had with his mentor about exploring the SNM arm of the study. It was an underexplored area—and one that aligned well his academic interests. At that point, understanding predictors of treatment response had never been examined in a controlled fashion, he says.
Advertisement
Their goal was to determine if any specific combinations of patient (muscle) responses at different electrodes amplitudes (stimulus strengths) were associated with improved outcomes that could guide future lead placement. The research team analyzed the intraoperative details of SNM from 161 women, including the responsive electrodes and differences in amplitudes along with response strengths. The 86% (N = 139) who showed significant improvements in stage 1 and ultimately elected for a permanent implant were followed for 24 months postoperatively.
But interpreting the data was not straightforward. “We had this massive dataset with a unique type of information that no one had really looked at before, and in working with our biostatistics groups, we devised a different way to analyze the data by considering how electrical stimulation interacts with nerves and whether or not there were patterns between this across the electrodes.”
Ultimately, their findings show that getting the best motor (muscle) responses from electrode 0, the most distal of the four electrodes, the tip of the implanted lead, resulted in overall better outcomes than a ‘best response’ at electrode 3, the proximal-most electrode.
“For implanting surgeons, the findings support the notion that more time should be spent on positioning and getting a good response from the distal-most electrode, mirroring lead placement to the anatomical curve of the nerve.”
Previous data on the topic is sparse and discourse has been varied, but Dr. Gill says the findings do corroborate what some SNM pioneers have asserted based on patient X-ray data. “Now we have some objective data to provide evidence about the importance of the positioning.”
Advertisement
What does it mean for patient care? Ultimately, Dr. Gill says, these findings may help guide decision-making in the initial testing phase of the device prior to permanent implant or explant.
“If you aren’t getting good clinical or urinary symptom responses despite testing during surgery suggesting the lead is in a good position, the patient may have a low likelihood of benefiting from the treatment – it would be reasonable to counsel them accordingly and set their expectations that another treatment may be needed,” he explains.
The study also calls attention to the technical nuance of urologic procedures. “Subtle differences in measurements or settings can have major impacts for patients and their outcomes. And for the highly technical treatments that we do, which continue to evolve and have become more complex, it’s important that we understand how to best apply and optimize them.”
Advertisement
Advertisement
Could it unlock the potential for new approaches to treatment?
Case study of radial-to-axillary nerve transfer for tumor-related deltoid nerve injury
Case illustrates essentials of the low-risk, high-potential procedure when paired with rehab
Increasing treatment options are extending the window for continued functional gains
Promising preclinical research indicates functional motor recovery is durable
New review distills insights from studies over the past decade
New care path supports obstetric patients with bladder dysfunction
Individual needs should be matched to technological features