Case is first of its kind to obviate heart transplant successfully
Heart transplantation seemed like the only option for the 3-week-old patient diagnosed with pulmonary atresia with intact ventricular septum (PA-IVS) and right ventricle-dependent coronary circulation (RVDCC). But quick thinking and a novel strategy to revascularize the RVDCC in the neonate with significant myocardial ischemia allowed the team to sidestep the need for a heart transplant altogether.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A team of Cleveland Clinic Children’s cardiac surgeons and cardiologists published a case report documenting their experience in The Journal of Thoracic and Cardiovascular Surgery.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/59a4d068-eac4-4ea3-b156-be793fe41ae9/23-CHP-3889480-CQD-Najm-AATS-Presentation-jpg)
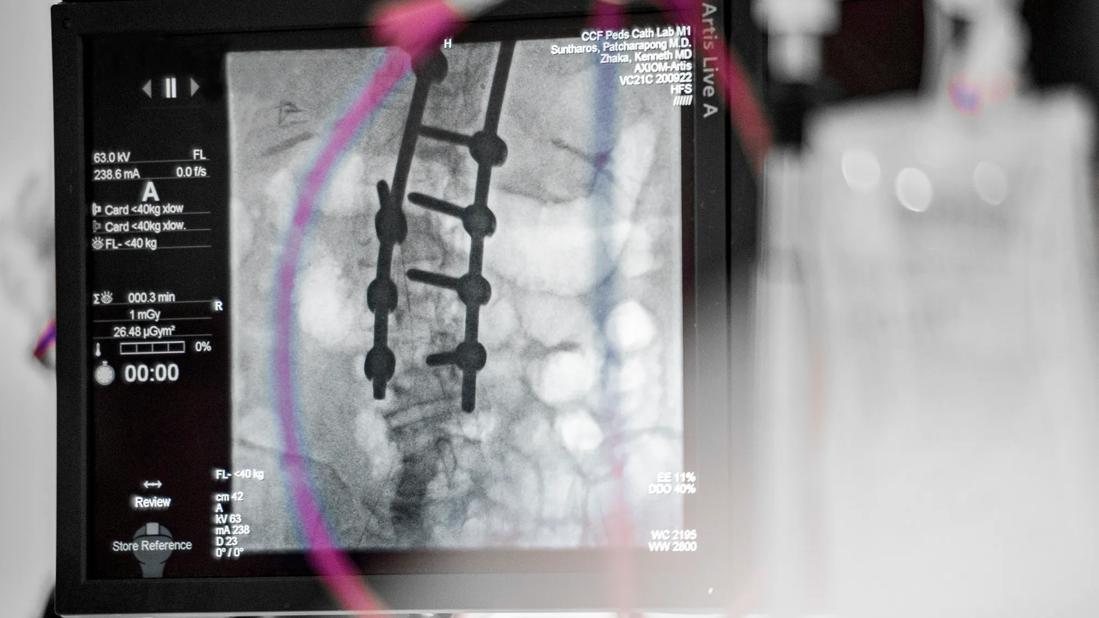
Right ventricular angiogram documenting extensive right ventricular-dependent coronary circulation.
PA-IVS is rare, accounting for less than 1% of congenital heart disease diagnoses and occurring in 4 to 8 per 100,000 live births. A subset of these patients is further complicated with RVDCC, progressive by nature and associated with a poor prognosis. Myocardial ischemia is commonly significant and difficult to stabilize in these patients.
The conventional pathway for treatment has been single-ventricle palliation without right ventricle (RV) decompression, and patients are typically listed for transplant in infancy. Still, the road to transplant can be difficult, and the risk of coronary compromise is high while awaiting transplant. The authors cite an 18% mortality rate in patients with PA-IVS and RVDCC within three months of systemic-to-pulmonary artery shunting.
The young Cleveland Clinic patient experienced many concerning physiologic and hemodynamic changes following birth, including a decrease in pulmonary vascular resistance, significant myocardial ischemia, along with ST segment changes and elevated troponin levels, which required intubation. The team had to act fast.
Stabilizing the circulation would take some “out-of-the-box thinking,” recalls Hani Najm, MD, Chair of Pediatric and Congenital Heart Surgery at Cleveland Clinic Children’s. “The fundamental problem was that the blood supply was coming out of the ventricle instead of the aorta, supplying the myocardium with blue blood. So, the question was, ‘How can we get red blood to that ventricle?’ and, ‘How do we isolate it from the blue blood and give it a higher pressure?’”
Advertisement
This is where his idea of the aortic-to-tricuspid valve (ATV) graft, “where you get better oxygenated blood from the aorta to the coronaries,” comes into play, notes Dr. Najm.
“Patients with PA-IVS and RVDCC have either occluded or stenotic proximal coronary arteries — or at least one of the coronary arteries. This means the blood supply to the myocardium needs to circulate through the small right ventricle then through the sinusoids to the coronary arteries and myocardium. The right ventricle has an inlet tricuspid valve. Therefore, the oxygenated blood can be brought to the tricuspid valve, so it flows through the ventricle then the coronary arteries,” Dr. Najm explains.
The plan Dr. Najm put forward to the team was to insert the standard modified Blalock-Taussig-Thomas (mBTT) shunt, then add the second shunt, or graft, from the ATV and, finally, insert a ventricular assist device to bridge the heart to recovery or to transplant.
He brought the idea to revascularize the RVDCC with the graft to a larger multidisciplinary group, which included Bradley Marino, MD, MPP, MSCE, MBA, Chair of Cardiology and Cardiovascular Medicine at Cleveland Clinic Children’s, who was closely involved in the patient’s care. The team of congenital cardiac surgeons and cardiologists agreed it was physiologically a good surgical alternative.
As planned, during the procedure, in addition to the ATV, Dr. Najm also inserted an mBTT shunt with a ventricular assist device to minimize potential risk and stabilize the circulation for the first 72 hours. The ventricular assist device was removed once her condition had stabilized.
Advertisement
The care team monitored the patient for about six months, and though her condition continued to improve, they kept her on the transplant list. When a slow decline in her oxygen saturation was observed, they devised a new plan. Dr. Najm performed the second stage of single-ventricle palliation: take down of the mBTT shunt, replacing it with a bidirectional cavopulmonary shunt and, simultaneously, upgrading the initial ATV graft to a 6 mm ringed polytetrafluoroethylene graft, which will likely remain intact until the child reaches adult life.
“Once that happened, the patient was extremely stable and doing well. We believe this physiology is better than a heart transplant,” emphasizes Dr. Najm. The child was doing so well, they were discharged home and removed from the transplant list shortly after the procedure. And, so far, she continues to do well.
While this extra graft was reported once in the literature, it ultimately led to heart transplant. This case is the first to obviate a heart transplant successfully.
Describing the mother’s joy, Dr. Najm beams, “She is over the moon. Her baby is home and effectively living a normal life.” The patient will continue to be followed by the heart failure team until progressing to the third and final phase of definitive treatment — the Fontan operation.
“Following the Fontan operation, her 15-year life expectancy is actually better than that of a heart transplant,” says Dr. Marino, “so this approach is a complete game-changer.”
Dr. Najm and colleagues provide proof of concept that this novel double shunt approach offers a solution for patients with PA-IVS and RVDCC, that may preclude the need for heart transplantation and offering a bridge to the next surgical stage.
Advertisement
Heart transplantation doesn’t come without a cost, Dr. Najm stresses. Further, timely access to transplant organs remains an issue in North America and is not a viable option for care in some parts of the world. This novel approach may not only prevent the need for transplant but may also improve longer-term outcomes in patients with RVDCC.
“It’s rare in your career to have the opportunity to work with a team that thinks outside the box to plan and execute a procedure to change the care paradigm for a group of patients at an extremely high risk for death,” says Dr. Marino.
Cleveland Clinic Children’s cardiology and heart surgery was recognized as a top 10 program from U.S. News & World Report in the 2023-2024 edition of “Best Children’s Hospitals.”
Image reprinted with permission under the Creative Commons CC-BY-NC-ND license. It originally appeared in the following: Najm HK, Costello JP, Karamlou T, Amdani S, Suntharos P, Marino B. Revascularization of coronary circulation in pulmonary atresia with intact ventricular septum and right ventricular-dependent coronary circulation. J Thorac Cardiovasc Surg. 2023 May 6:S0022-5223(23)00330-6. doi: 10.1016/j.jtcvs.2023.04.007.
Advertisement
Advertisement

Innovative hardware and AI algorithms aim to detect cardiovascular decline sooner

Experts advise thorough assessment of right ventricle and reinforcement of tricuspid valve

Reproducible technique uses native recipient tissue, avoiding risks of complex baffles

A reliable and reproducible alternative to conventional reimplantation and coronary unroofing

Program will support family-centered congenital heart disease care and staff educational opportunities

Case provides proof of concept, prevents need for future heart transplant

Pre and post-surgical CEEG in infants undergoing congenital heart surgery offers the potential for minimizing long-term neurodevelopmental injury

Science advisory examines challenges, ethical considerations and future directions