More accurate than existing noninvasive tests
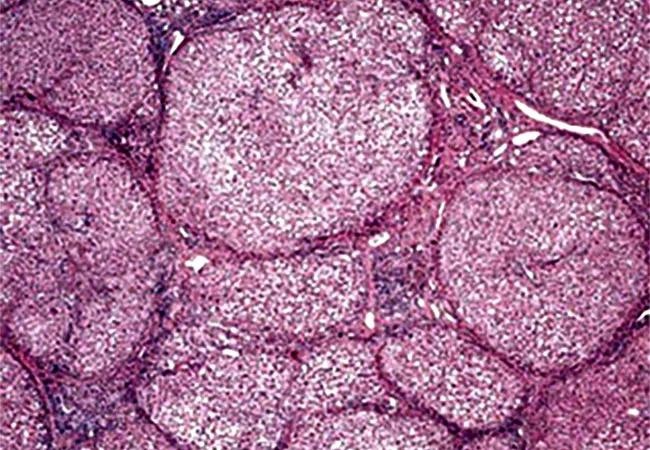
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/7dabc8f9-0211-4bea-81fb-f56593daa794/650x450-Non-Alcoholic-Fatty-Liver-Disease_jpg)
Nonalcoholic cirrhosis
A team of Cleveland Clinic researchers developed a novel machine learning model that correctly identifies the majority of non-alcoholic fatty liver disease (NAFLD) patients with advanced fibrosis who are indeterminate by the Fibrosis-4 (FIB-4) Index.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Advanced fibrosis in NAFLD is the most important predictor of mortality and liver-related morbidity. Of the noninvasive tests developed to detect fibrosis, FIB-4 is a commonly used index. However, a significant number of patients are classified as indeterminate and will require further testing and/or liver biopsy.
“Identification of liver fibrosis is crucial to guide patient management in NAFLD, which affects 30% of the world population,” explains study author Manik Aggarwal, MD, an internal medicine resident at Cleveland Clinic. “FIB-4 is a commonly used index to identify fibrosis; however, when using FIB-4, almost 40% of patients fall into the indeterminate category and require further testing, thus increasing cost and risk of morbidity and mortality.
“Machine learning has emerged as a novel tool for predictive modelling since it is able to identify complex relationships between parameters,” he continues. “So, we designed a study to see if a machine learning model can identify patients with advanced liver fibrosis who were indeterminate by the FIB-4 index.”
The study included 960 histologically confirmed NAFLD patients at Cleveland Clinic with a mean age of 50.7 years and BMI of 40.8 Kg/m2. The researchers used the NASH Clinical Research Network (NASH-CRN) criteria to score all biopsies, and advanced fibrosis was defined as fibrosis stage ≥ 3.
Thirty-six covariates were considered when building the machine learning model, including demographic, clinical and commonly measured laboratory parameters within three months of liver biopsy. The researchers built the model by segregating 20% of data into a blinded validation cohort and using the remaining 80% of data to iteratively train and test. The final model incorporated 13 features to guide the prediction of advanced fibrosis.
Advertisement
The train-test cohort (N = 768) had an area under the curve (AUC) of 0.83, and the validation cohort (N = 192) had an AUC of 0.80, according to the study authors, who report that these three cohorts had sensitivity/specificity for diagnosing advanced fibrosis of 0.86/0.67, 0.84/0.59 and 0.84/0.64.
“The machine learning model was superior to FIB-4 in diagnosing advanced fibrosis. In the validation set, the model correctly classified 71% of patients as either having or not having advanced fibrosis whereas FIB-4 index correctly identified 60% of cases,” says Dr. Aggarwal. “Thirty percent of patients were indeterminate when using FIB-4 index in the validation set. The model was able to correctly identify 80% of cases with advanced fibrosis in this subgroup, which would otherwise have required a liver biopsy.”
This machine learning model is a novel solution to the current problem with noninvasive tests and reduces the need for additional evaluation. This model, which uses covariates available at all clinical centers, has wide applicability. The study authors note that prospective studies are needed with larger cohorts to assess validity.
“Our machine learning model can be easily implemented in the electronic medical record and identify patients with advanced liver biopsy using routinely recorded clinical and lab parameters,” emphasizes Arthur McCullough, MD, staff in the Department of Gastroenterology, Hepatology & Nutrition at Cleveland Clinic.
“It can prevent liver biopsies in up to 80% of cases that were originally indeterminate by FIB-4,” he concludes. “As NAFLD affects 30% of the population, avoiding the need for costlier and more invasive tests can decrease cost, improve patient safety and help focus our attention to those patients that require closer monitoring and care.”
Advertisement
Advertisement
Benefits of neoadjuvant immunotherapy reflect emerging standard of care
Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence
Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors
Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling
Potentially cost-effective addition to standard GERD management in post-transplant patients
Findings could help clinicians make more informed decisions about medication recommendations
Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care
Retrospective analysis looks at data from more than 5000 patients across 40 years