Treating OSA could improve quality of life for liver disease patients
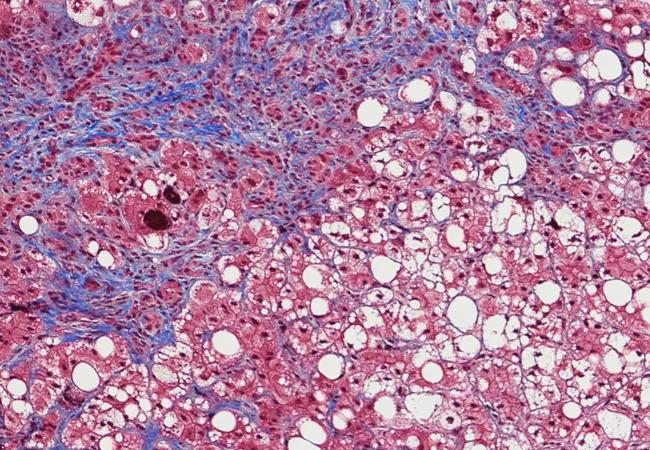
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/7f7338e5-ecce-4f02-ad10-6b3e9de5826e/17-DDI-3953-Fibrosis-CQD_jpg)
17-DDI-3953-Fibrosis-CQD
Nonalcoholic fatty liver disease (NAFLD) is an epidemic in the U.S., affecting 30 percent of the adult population. A percentage of patients with nonalcoholic steatohepatitis (NASH), an advanced form of NAFLD, will progress to cirrhosis without consuming a drop of alcohol. This type of cirrhosis is the third most common cause of liver transplantation in the U.S.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
It’s no surprise that intense frustration and unanswered questions often follow a nonalcoholic steatohepatitis diagnosis. Patients without a history of alcohol abuse may wonder how they could have developed NAFLD. Physicians may also be discouraged by the lack of FDA-approved treatments for this condition.
To improve the state of the liver, some hepatologic experts treat the comorbidities of NAFLD, such as obesity, high blood pressure and diabetes. Cleveland Clinic researchers recently studied the potential link between nonalcoholic steatohepatitis and obstructive sleep apnea (OSA), a possible comorbidity.
Presented at the annual conference of the American Association for the Study of Liver Diseases (AASLD), the study revealed for the first time that patients with OSA are three times more likely to have NASH — compared with patients who don’t have OSA.
Led by Mohammad Maysara Asfari, MD, and Arthur McCullough, MD, the researchers proved that OSA is an independent risk factor for developing NASH, a discovery that will likely increase the number of viable treatment options for patients with nonalcoholic steatohepatitis.
In the past, medical researchers conducted small studies in animals as well as studies involving bariatric surgery candidates to analyze the link between OSA and NASH. While some researchers found a connection between oxygen levels in the blood and liver enzyme levels, most published literature offered conflicting messages and conclusions.
Dr. Asfari’s team analyzed data from the 2012 Nationwide Inpatient Sample, a database of 30.7 million patients who were admitted and discharged from community hospitals in the U.S. “Using this database was particularly valuable since it provided a true sample of the general population rather than a subset of patients who were treated at research-based medical centers,” notes Dr. McCullough.
Advertisement
The researchers identified 1.5 million adults between the ages of 18 and 90 who had OSA. After adjusting for other comorbidities and risk factors, the researchers found that the OSA patients were three times more likely to have NASH.
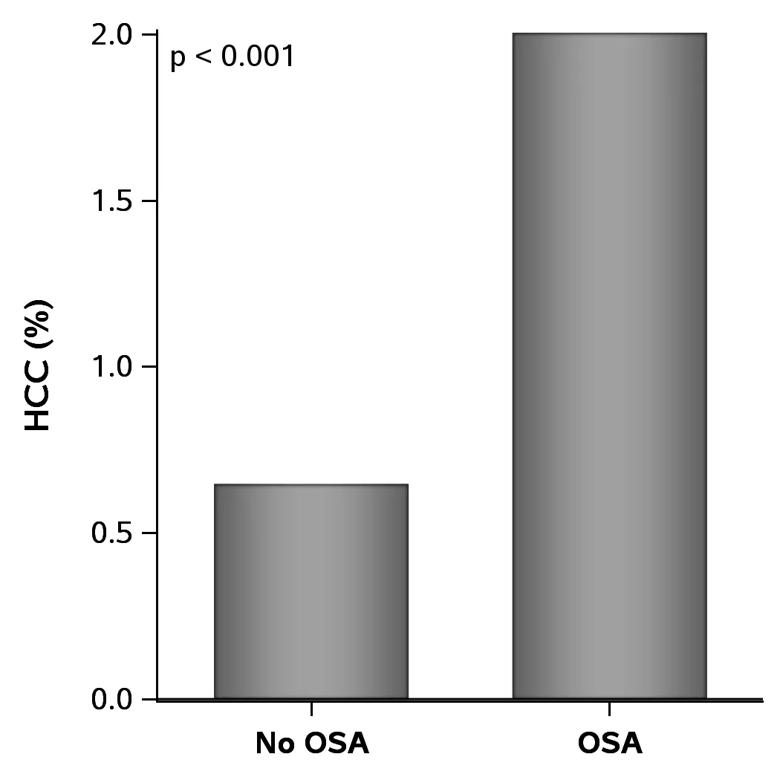
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/38a7b510-2787-41ef-bedf-a1cb172eda65/1_png)
Figure 1. Prevalence of NASH in adult subjects with and without OSA.
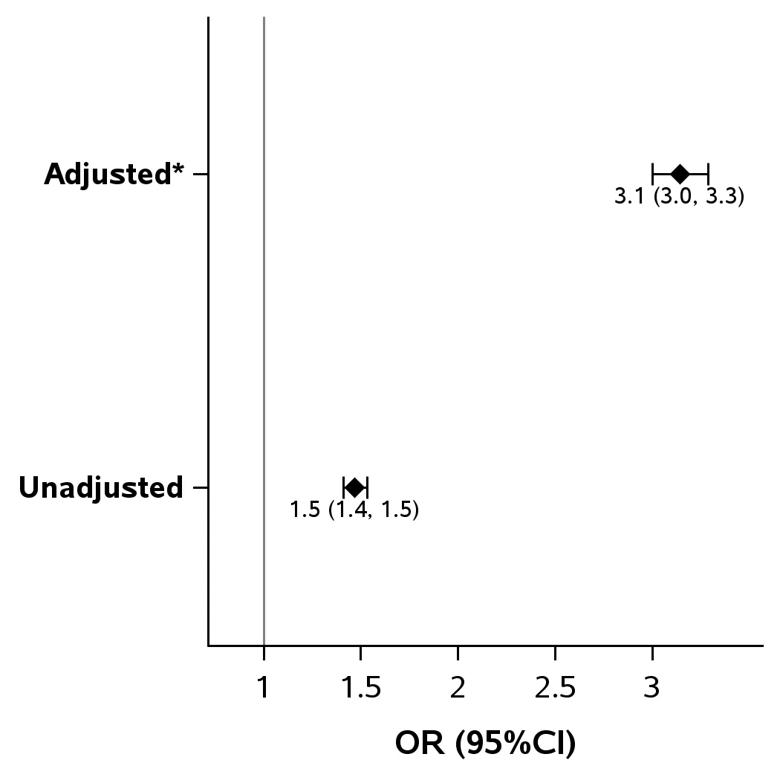
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/14dbb985-c455-42c5-9cd1-0722f3155634/2_png)
Figure 2. Association between OSA and NASH in adult subjects. (*Adjusted for obesity, diabetes, hypertension, dyslipidemia, metabolic syndrome and Charlson comorbidity index).
Now that OSA has been identified as an independent risk factor for nonalcoholic steatohepatitis, physicians can start treating OSA in patients with fatty liver disease. “Previous research suggests that the continuous positive airway pressure (CPAP) machine helps improve liver enzymes, which could make it easier to manage fatty liver disease,” says Dr. McCullough. “Regardless of the effect on the liver, the patient’s quality of life is likely to improve with OSA treatment. Once these patients start using the CPAP machine, they tend to have more energy, lower blood pressure and reduced insulin resistance.”
Dr. McCullough hopes that Cleveland Clinic’s latest research will encourage physicians to talk with their patients about sleep apnea, whether it’s referring them to a sleep center or recommending CPAP treatment. “Even if patients with nonalcoholic steatohepatitis already use a CPAP machine, the device could be old or cause discomfort,” he says. “We have new and enhanced devices that can improve their quality of life — and hopefully their liver function.”
Advertisement
According to Dr. McCullough, the next steps in the process involve studying the effect of CPAP treatment on patients with OSA and nonalcoholic steatohepatitis and measuring the true impact on liver disease. In addition, Cleveland Clinic researchers have plans to study a small molecule that inhibits hypoxia-inducible factor, a protein complex that is reduced by sleep apnea and known to cause liver injury.
Advertisement
Advertisement
Benefits of neoadjuvant immunotherapy reflect emerging standard of care
Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence
Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors
Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling
Potentially cost-effective addition to standard GERD management in post-transplant patients
Findings could help clinicians make more informed decisions about medication recommendations
Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care
Retrospective analysis looks at data from more than 5000 patients across 40 years