Single-arm, open-label study offers proof of concept for MSC-NTF cells
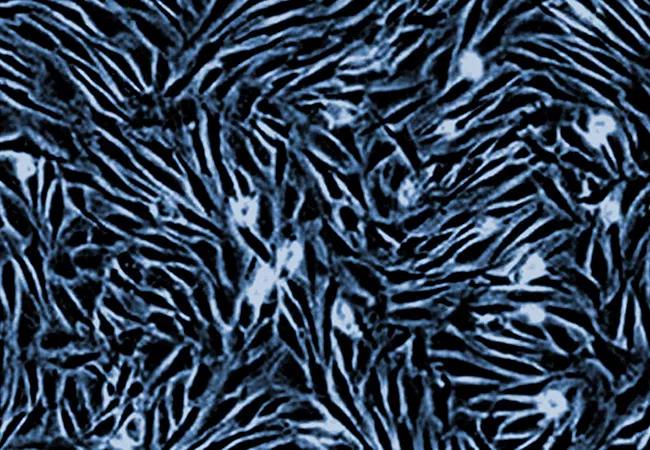
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5a65f763-2d62-473d-96ca-9e02b5f2c446/22-NEU-3222062_mesenchymal-stem-cells_650x450_jpg)
22-NEU-3222062_mesenchymal-stem-cells_650x450
In patients with progressive multiple sclerosis (MS), accumulating central nervous system injury leads to damage of both white and gray matter in the brain. The result is functional impairments for which no effective reparative therapies are currently available.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
New findings from a phase 2 study provide preliminary evidence on the safety and potential efficacy of using autologous mesenchymal stem cells that secrete neurotrophic factors (MSC-NTF cells) to treat patients with progressive MS. The results from the study, published online in Multiple Sclerosis Journal, reflect experience in a small population in an open-label setting without a placebo group.
“The efficacy data offer promising biological and clinical signals of a treatment effect, but because of the lack of a comparator group, they should be interpreted with caution,” says lead author Jeffrey Cohen, MD, Director of the Experimental Therapeutics Program in Cleveland Clinic’s Mellen Center for Multiple Sclerosis Treatment and Research. “These preliminary results need to be confirmed in a placebo-controlled trial.”
MSC-NTF cells are produced from autologous, bone marrow-derived MSCs that are expanded and differentiated in culture. The MSCs are converted into MSC-NTF cells by cultivating them under conditions that induce secretion of high levels of NTFs and immunomodulatory cytokines. Successful evaluation of MSC-NTF in animal models relevant to progressive MS led to initial assessment in humans, with intrathecal administration eventually chosen to enable direct delivery of NTFs to the central nervous system.
The phase 2 study was conducted from March 2019 to March 2021 at four U.S. academic centers, including Cleveland Clinic. Twenty adults were enrolled, all of whom had primary/secondary progressive MS, no relapse 6 months prior to screening, a baseline Expanded Disability Status Scale (EDSS) score of 3.0 to 6.5, and a timed 25-foot walk speed (T25FW) of ≤ 60 seconds.
Advertisement
Participants were allowed to continue taking a stable dose of an approved disease-modifying therapy. After a pretreatment period of approximately 10 weeks during which the cells were cultured, autologous MSC-NTF cells were administered intrathecally at weeks 0, 8 and 16, followed by a 12-week post-treatment observation period.
Eighteen participants (10 women, eight men) with a mean EDSS score of 5.4 ± 1.3 and a mean age of 47.4 ± 9.6 years ultimately were treated with MSC-NTF cells. Seventeen received all three treatments, and one received two treatments.
The primary endpoint was safety, assessed in terms of incidence of treatment-emergent adverse events (TEAEs) and clinically relevant changes in vital signs, need for concomitant medications, clinical laboratory assessments and physical/neurologic testing. T2 lesion status at baseline and at study’s end was evaluated with brain MRI.
No deaths or adverse events related to worsening of MS occurred, and no clinically significant changes in safety lab results or vital signs were reported.
During the study, two patients developed symptoms of low back and leg pain accompanied by characteristic clumping of lumbar nerve roots on MRI, consistent with arachnoiditis. In both patients, symptoms developed after one of the three intrathecal treatments. In one patient, the symptoms occurred after the second treatment and resolved after administration of epidural cortisone injections and analgesics, which enabled completion of the third treatment with no complications. In the second patient, the apparent arachnoiditis occurred after the third intrathecal administration and did not fully resolve with treatment.
Advertisement
Two study participants were hospitalized for serious TEAEs. One was the second patient with arachnoiditis noted above, who withdrew from the study. The other reported nonspecific symptoms — anxiety and dizziness that led to study withdrawal — after their second treatment.
No other safety signals were seen, and there was no change in brain T2 lesion volume or count in brain FLAIR MRI measures over 28 weeks to suggest disease activation.
Clinical response was prespecified as an improvement of ≥ 25% from baseline (considered a clinically meaningful change) in the T25FW or the 9-hole peg test at week 28. Efficacy was also assessed in terms of improvement in scores on the EDSS, the Symbol Digit Modalities Test (SDMT), the low-contrast letter acuity test (LCLA) and the 12-item Multiple Sclerosis Walking Scale (MSWS-12). The efficacy outcomes in study participants were compared with those of a prespecified matched group of 48 patients with progressive MS from the CLIMB Study registry.
Clinical response was achieved by 19% of study participants compared with 4% of matched CLIMB registry patients. Additionally, from 27% to 67% of study participants showed clinically meaningful improvements from baseline in scores on the LCLA, MSWS-12 and SDMT; no patients with a baseline EDSS score ≤ 5.5 showed improvement ≥ 1.0, although 30% of patients with a baseline EDSS score > 5.5 showed improvement ≥ 0.5.
Additionally, treatment consistently resulted in increases in cerebrospinal fluid neuroprotective factors (VEGF-A, HGF, NCAM-1, follistatin, LIF and fetuin-A) as well as reductions in inflammatory biomarkers (MCP-1, sCD27, SDF-1 and osteopontin).
Advertisement
“The combined activity of MSC-NTF cells in immunomodulation and neuroprotection may be relevant to progressive MS,” says Dr. Cohen, “and intrathecal delivery of the therapy may offer an advantage by directly addressing compartmentalized inflammation and/or failure of neuroprotective mechanisms. It is not possible, however, to extrapolate observations in this study to patients with progressive MS experiencing clinical or MRI disease activity. We look forward to further studies of this interesting therapeutic approach.”
The study was funded by Brainstorm Cell Therapeutics, which is developing the MSC-NTF cell therapy.
Advertisement
Advertisement
Mixed results from phase 2 CALLIPER trial of novel dual-action compound
A co-author of the new recommendations shares the updates you need to know
Rebound risk is shaped by patient characteristics and mechanism of action of current DMT
First-of-kind prediction model demonstrates high consistency across internal and external validation
Real-world study also finds no significant rise in ocrelizumab-related risk with advanced age
Machine learning study associates discrete neuropsychological testing profiles with neurodegeneration
This MRI marker of inflammation can help differentiate MS from mimics early in the disease
Focuses include real-world research, expanding access and more