Patient is smiling again

By Michael P. Horan, MD, DDS, PhD, and Sanjay Karunagaran, BDS, DDS, MSD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Benign oral and maxillofacial pathology requiring resective jaw surgery is rare in the general population. However, these patients are becoming relatively common in tertiary care centers like Cleveland Clinic. Why? Because individual physicians in the community often indicate that they lack the resources and the time to provide comprehensive care to these unique individuals. Continuity of care is also affected as it is frequently difficult to enlist other medical specialists in the community to engage in care of these patients. This often results in early referral to large academic centers and hospitals where specialists and subspecialists are in abundance.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/0800d6ff-03de-48e7-a078-d2848160a09a/17-ENT-4070-Horan-Inset-Image-01_jpg)
Figure 1
Here, we share the case of a 41-year-old male from Kuwait who presented with a large multilocular, expansile lesion in the mandible (Figure 1). The lesion was noted to cross the midline and, when biopsied, was consistent with a central giant cell granuloma. Given the size of the lesion, the patient elected to undergo resective jaw surgery versus more conservative measures. Being that the lesion was less than 6 cm in length, it was determined that the patient would benefit from microvascular reconstruction with a free fibula flap.
Medical modeling was performed and a custom plate was fabricated for the case (Figure 2). The patient subsequently underwent resection of the central giant cell granuloma (Figure 3) by oral and maxillofacial surgery and microvascular reconstruction by the Head & Neck Surgery team (Figure 4). After an uneventful recovery, the patient was ready to have his mandibular dentition replaced.
Advertisement
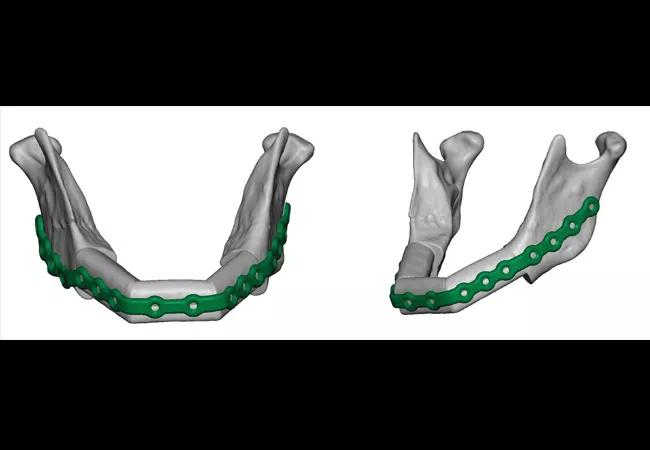
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a246c2a0-9c0a-434a-b37c-ca0150b5421e/17-ENT-4070-Horan-Inset-Image-02_jpg)
Figure 2

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/f65354c1-a6ba-476b-894f-e79860c9ad14/17-ENT-4070-Horan-Inset-Image-03_jpg)
Figure 3

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/39ab2ca2-8458-4b23-b65a-e8e2cbe7eda5/17-ENT-4070-Horan-Inset-Image-04_jpg)
Figure 4
The patient presented to the Maxillofacial Prosthodontic Clinic for evaluation following clearance from his surgeon who performed the reconstruction. A comprehensive treatment plan was custom-tailored to meet the patient’s need. He wished to have a fixed versus removable prosthesis, so his treatment plan called for implant reconstruction of the mandible with a fixed complete denture. The patient subsequently underwent surgical placement of six bone-level implants into the reconstructed mandible (Figure 5). These implants were allowed to heal for a period of several months prior to uncovering and placement of healing abutments. Once the healing abutments were placed, care of the patient was turned over to our prosthodontist.
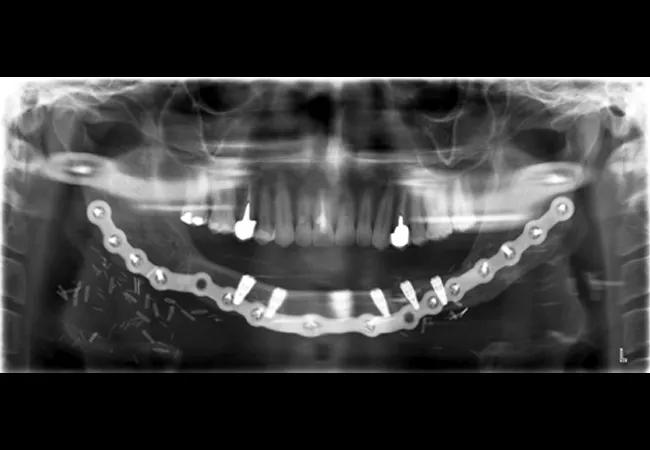
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/839f7bdb-cf16-4e33-9e4f-9048e287c6c4/17-ENT-4070-Horan-Inset-Image-05_jpg)
Figure 5
On presentation for prosthetic reconstruction, the thickness of the fibula free flap revealed that standard metal impression copings were unusable as they were buried under the free flap. Special abutments were connected to implants in order to traverse the free flap tissue transmucosally for prosthetic connection and correction of any minor angulation issues with the implants. Impressions of the implants were made to capture all implant positions.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/468ee5c4-f15d-494e-96a6-64e8a2c05280/17-ENT-4070-Horan-Inset-Image-06_jpg)
Figure 6
A verification index (Figure 6) was then transferred intraorally to check accuracy of the implants captured. Next, a mandibular fixed complete denture prosthesis was designed and fabricated based on where the patient’s bite would have been prior to surgery. The inserted prosthesis helped restore the patient and make up for the lost bone, tissue and tooth height (figure 7). This patient left for Kuwait to be with his family in very high spirits, and a two-year treatment plan finally came to fruition. His family can see him smiling once again.
Advertisement

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/4d1facc2-e18b-43a9-b0a4-a9eef91eb50f/17-ENT-4070-Horan-Inset-Image-07_jpg)
Figure 7
Dr. Horan is Section Head of Oral and Maxillofacial Surgery. He can be reached at horanm@ccf.org. Dr. Karunagaran is a prosthodontist in the Department of Dentistry.
Advertisement
Advertisement

Analysis of HNSCC patients shows HPV status to be predictive of higher abundance of oncobacteria within the tumor

Case study illustrates the potential of a dual-subspecialist approach

Evidence-based recommendations for balancing cancer control with quality of life

Study shows no negative impact for individuals with better contralateral ear performance

HNS device offers new solution for those struggling with CPAP

Patient with cerebral palsy undergoes life-saving tumor resection

Specialists are increasingly relying on otolaryngologists for evaluation and treatment of the complex condition

Detailed surgical process uncovers extensive middle ear damage causing severe pain and pressure.