The decision to use 223-radium, and an outcome that exceeded expectations
When a 24-year-old patient arrived at Cleveland Clinic in March 2021 after a referral from another center, he could barely walk.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
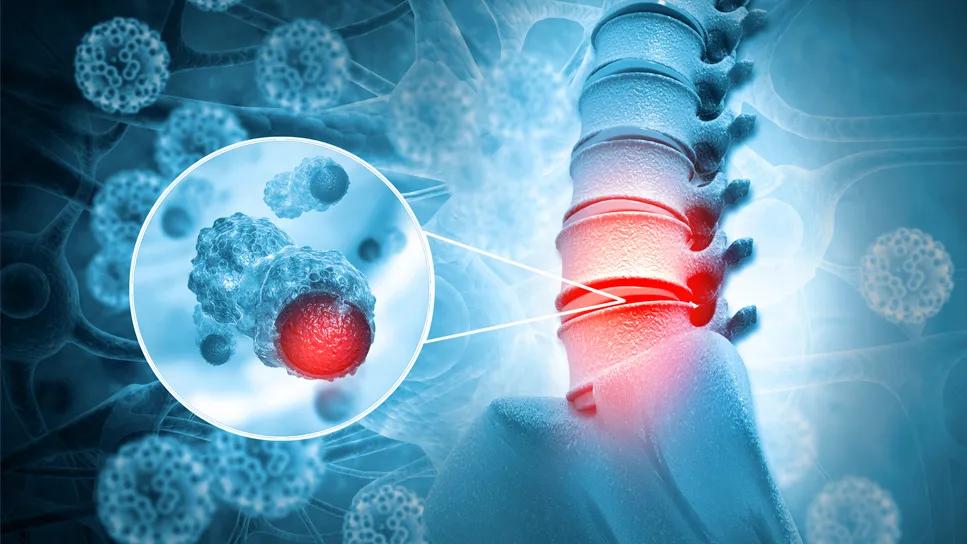
He had been diagnosed with paraspinal osteosarcoma almost exactly one year prior. Osteosarcoma of the spine is rare, and while treatment modalities have improved, the prognosis is still typically poor. A combination of complete resection, chemotherapy and radiation therapy is often indicated to achieve a good outcome.
He had already received a standard chemotherapy regimen at the previous center that included cisplatin plus doxorubicin, high-dose methotrexate, and ifosfamide-mesna with etoposide; however, the tumor continued to progress.
Peter M. Anderson, MD, PhD, a hematologist/oncologist at Cleveland Clinic Children’s, recalls when he first became involved in the case. It was presented at a sarcoma tumor board conference in late 2020 to a multidisciplinary team of Cleveland Clinic musculoskeletal radiologists, sarcoma pathologists, medical and radiation oncologists, and a team of orthopedic, spine and thoracic surgeons.
“These are very talented surgeons, who are used to working together to do very difficult surgeries. And their take on it was that they could do the surgery, but it would likely leave positive margins with possibly devastating side effects,” says Dr. Anderson. So, the team continued to weigh their options.
“Solid tumors, particularly osteosarcoma, always need some form of local control,” he says.
But local control would be difficult, given the location of the tumor. The mass was situated near his upper thoracic spine, spinal cord, and the left upper lobe of his lung. Complete surgical resection for this advanced malignancy would be nearly impossible, and too much radiation could potentially damage his spinal cord.
Advertisement
Dr. Anderson considered his clinical experiences with alpha-emitting bone-seeking radiopharmaceuticals, most recently, 223-radium (Xofigo). In 2020, he published the first series of patients with metastatic osteosarcoma who have been treated with 223-radium in combination with other agents, including denosumab and chemotherapy. He thought the patient could be a good candidate for the drug.
Xofigo was developed more than a decade ago with the goal of limiting bone marrow toxicity when treating bone metastases. The team of scientists conducted the randomized controlled trial in patients with resistant prostate cancer and bone metastases. Interim results of the drug’s efficacy were associated with such strong outcomes in one of the study’s arms that investigators actually halted the study to be able to administer the drug to the control group, Dr. Anderson explains. The analysis was published in the New England Journal of Medicine.
“Radium, at a short distance, can provide a ‘roundhouse right’ to a tumor cell. It can also cause a DNA double-strand break, which is hard to repair, but it happens at such short distances—we are talking 0.1 mm — so, it’s not going hit a lot of important things nearby, which, in this case, was the spinal cord and lung,” he says.
The team and the patient agreed to move forward with the plan.
Because 223-radium is not currently FDA approved for treating osteosarcoma, despite emerging data demonstrating its safety and efficacy, its use was not approved by the patient’s insurance. Dr. Anderson appealed—successfully—with a personal letter and picture of the patient.
Advertisement
He had been working closely with the patient’s local treating physician since first getting involved in the case. Together the care teams developed a strategy to make treatment, and the travel it entailed, more efficient.
Under the care of Dr. Anderson, the patient would receive the radium one day, followed by a gemcitabine infusion the next day. He would then return home, and his counts would be monitored by the team at the local center. He would return to Cleveland Clinic the following month, repeating this pattern for six total rounds of treatment.
“Before the first dose, he could barely walk. He used a cane, and you could just see he was losing strength and would probably become paralyzed from the chest down,” reflects Dr. Anderson. “But with time, he just kept getting better. And at the end of the six doses, we said, ‘Wow, what can we do next?’”
They decided on six months of oral cyclophosphamide since he had tolerated the ifosfamide well previously, and because both cyclophosphamide and ifosfamide are metabolized to the same active drug, Dr. Anderson suspected it would enable a “more durable remission.” And it did.
His last cycle of treatment was in September 2021, just a few months short of a year since Dr. Anderson first became involved in the patient’s care. The tumor had shrunk considerably, and the patient completely regained his functional mobility—and then some. Dr. Anderson smiles recalling a video the patient captured of his tre flip, an advanced skateboarding trick. He is also an active rock climber and skydiver.
Advertisement
At the conclusion of treatment, Dr. Anderson reported an update on outcomes at tumor board to the same team that had discussed the case in late 2020. “It was a joy to share the outcome and also that they made the right decision not to do the surgery and instead to try the 223-radium, a ‘roundhouse right’ alpha emitter.”
He continues, “If he relapses, hopefully, it’s just in a small spot, which can be treated either with SBRT, or a very limited surgery, but I am hopeful that he won’t relapse at all.”
“This is the kind of thing that just makes you smile for a while and say, ‘This is why I do what I do: teamwork makes the dream work!”
Advertisement
Advertisement

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists

Structured interventions enhance sleep, safety and caregiver resiliency in high-acuity units