Case report: Primary laryngeal NK/T-cell lymphoma
Natural killer (NK)/T-Cell lymphoma is a subtype of non-Hodgkin lymphoma (NHL) that comprises 2-20% of NHL cases. Most NHLs involve the lymph nodes, with an estimated 10-35% extranodal, mostly involving the head and neck. The larynx is the primary site in less than 1% of all hematopoietic neoplasms, with lymphoma the second most common after plasmacytoma.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Since 2016, only 31 cases of primary laryngeal (NK)/T-Cell lymphoma have been reported in the English, Chinese and Japanese literature. There is very little in the literature describing the management of treatment-related morbidities. Laryngeal NK/T-Cell lymphoma is more prevalent in Asian countries and in men with a median age of 40 to 50. The nasal subtype of lymphoma is very aggressive and strongly associated with Epstein-Barr virus infection. The presentation can include dysphonia, globus sensation, weight loss, stridor and dysphagia. The prognosis is poor.
In 2016, the first patient with primary laryngeal NK/T-Cell lymphoma was treated at Cleveland Clinic. The case is reported in the American Journal of Otolaryngology.
The patient was a 27-year-old female from Palestine with no significant medical history. She initially presented with a three-week history of flu-like symptoms including sore throat, myalgia and insidious nasal congestion.
Her condition worsened and she developed complete bilateral nasal blockage, dysphagia and odynophagia, and subjective fevers and chills. Antibiotics were prescribed but were not effective.
After hospital admission for a 103.1° F temperature, she had a CT/PE, which was positive for multifocal centrilobular ground-glass nodules, concentric subglottic tracheal narrowing and splenomegaly. She underwent an extensive rheumatologic, hematologic and infectious workup that was negative.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/20c5a34a-0d0f-4d39-9800-9460a235467c/Figure-1-CT-neck-w-IV-contrast-pre-treatment-axial_jpg)
Figure 1. CT of neck with IV contrast, pre-treatment (axial).
Flexible laryngoscopic and bronchoscopic examinations with biopsies exhibited a diffuse supraglottic and glottis exophytic, “heaped-up” infiltration; limited vocal cord motion; and extension of the process to the subglottic trachea causing an airway narrowing to 3 mm with an otherwise normal pulmonary scan.
Advertisement
The pathology revealed NK/T-Cell lymphoma with PET/CT confirming nasopharyngeal and laryngeal involvement but sparing the brain and distant structures.
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b9382128-7f63-4990-a9ae-caad896b988c/Figure-2-PET-CT-pre-treatment-sagittal_jpg)
Figure 2. PET/CT, pre-treatment (sagittal).
“The location of the lymphoma in the larynx is the greatest challenge in addressing this disease. It made the patient’s breathing and communication very difficult,” says Paul C. Bryson, MD, Director of the Cleveland Clinic Voice Center and Section Head of Laryngology.
Treatment at Cleveland Clinic was multidisciplinary, with medical oncology administering therapy and otolaryngology managing airway breathing and swallowing. The patient received four rounds of SMILE (dexamethasone, methotrexate, ifosfamide, l-asparaginase and etoposide) chemotherapy and subsequent radiotherapy with 50 Gy in 25 fractions. During treatment, she required a tracheostomy. “The disease is very destructive to the larynx. The surgeon should plan on a tracheostomy,” says Dr. Bryson.
Following treatment, flexible laryngoscopic examination revealed complete glottis stenosis with alteration of the laryngeal anatomy and a pin-hole aperture seen posteriorly through the tracheostomy.
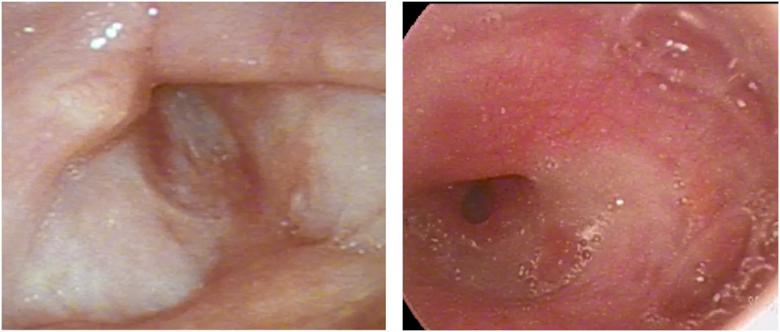
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/cfe40a45-a0a4-439f-a06e-c076b3d40f2c/gure-3-Flexible-laryngoscopy-of-larynx-post-treatment-from-a-A-superior-view-and-B-inferior-view_jpg)
Figure 3. Flexible laryngoscopy of larynx post-treatment from a (A) superior view and (B) inferior view.
Two dilation procedures improved her airway considerably and allowed for complete removal of the tracheostomy tube.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/935380e8-b05c-4a71-b333-96796ebe9d13/gure-4-Flex-laryngoscopy-of-the-larynx-post-operative-from-a-A-superior-view-and-B-inferior-view_jpg)
Figure 4. Flexible laryngoscopy of the larynx, post-operatively, from a (A) superior view and (B) inferior view.
The patient returned to Israel where she is being managed by a local otolaryngologist. At last report, she had been disease free for more than a year but has persistent supraglottic and glottis scar. She required another tracheostomy due to restenosis at the tracheostomy site. In addition, she underwent tracheal reconstruction with stent and skin graft with results pending.
Advertisement
“The remission from lymphoma is encouraging but the post-treatment morbidity is the biggest disappointment. The chemotherapy and radiotherapy make wound healing and long-term scar formation difficult to treat. The prognosis for tracheostomy-free survival and normal communication is limited,” says Dr. Bryson.
As genetic information is increasingly used to characterize tumors and guide lymphoma treatment, it is possible that the chemotherapy regimen for primary laryngeal NK/T-Cell lymphoma could be de-escalated, or more precisely targeted, to minimize morbidity.
Please note: Images used with permission from Elsevier. They originally appeared in the following journal article: Meleca JB, Hanick A, Lamarre E, Bryson PC. Post-treatment sequelae and management of primary laryngeal NK/T-cell lymphoma: A case report. Am J Otolarngol. 2018 July:39(6):891-784.
Advertisement
Advertisement

Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors