Study of a family with Cowden Syndrome, thyroid cancer
Charis Eng, MD, PhD, and her team have discovered that a faulty, rarely studied gene called USF3 may predispose individuals to thyroid cancer. They recently published this discovery in Human Molecular Genetics.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
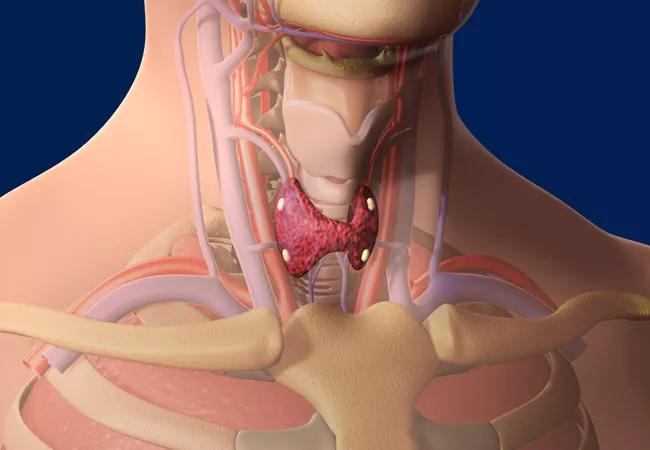
Differentiated thyroid cancer (DTC) is the fastest rising incident cancer in the US. Although epidemiologic studies show that thyroid cancer is the most familial of all solid tumors, the known genes predisposing to DTC do not account for all the familial nature of DTC.
Dr. Eng is an expert in the study of Cowden syndrome (CS), an autosomal disorder that predisposes individuals to breast, thyroid and other epithelial cancers. Patients with CS develop noncancerous growths, called hamartomas, which can appear on the skin, in mucous membranes and in the intestinal tract. This disease affects at least one in 200,000 people. With up to 50 percent of CS patients testing negative for all known genetic mutations, the syndrome remains an underdiagnosed and difficult-to-recognize condition.
Dr. Eng’s team in the Genomic Medicine Institute discovered a novel genetic cause for CS/CS-like disorder by focusing on thyroid cancer predisposition in a family with CS and thyroid cancer. Using a combined family-based, whole-genome sequencing strategy, they identified an inherited variant (a compound heterozygous deletion) in USF3 in a subset of heritable CS/CS-like patients.
The deletion or malfunction of USF3 causes a very stressful microenvironment, including metabolic issues and structural instability of the cell. The metabolic issues stem from an enhanced epithelial-to-mesenchymal transition (EMT) signature, which is known to cause tumor progression and metastasis. The cell surface is also compromised from necrosis-like features and impaired respiratory capacity, all of which are hallmarks of cancer.
Advertisement
Additionally, of the nine family members studied, seven were affected with papillary thyroid cancer. Dr. Eng’s team found the USF3 deletion in those family members affected with thyroid cancer and thus suspected that USF3 may be involved in a predisposition toward thyroid cancer.
The researchers also discovered a potential therapeutic strategy given USF3’s glutamine-dependent cell survival advantage. Like most tumor cells, USF3-deficient cells actually can survive low-glucose conditions, but this survival requires glutamine supplement, suggesting that glutamine removal might have therapeutic potential in patients with USF3-related thyroid cancer.
The discovery of this cancer predisposing gene will facilitate predictive genetic testing, risk assessment, genetic counseling and clinical management of the disease. Currently there is no genetic test for USF3, but these findings could improve therapeutic and preventive interventions for both sporadic cancer and cancer predisposition in similar mechanisms.
Advertisement
Advertisement

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists

Structured interventions enhance sleep, safety and caregiver resiliency in high-acuity units