Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/64734313-0058-4c3f-9e6c-4d62273b4006/590x-Inset-Interop-Brain-Tumor_jpg)
590x-Inset-Interop-Brain-Tumor
The skull base is one of the human body’s most complex anatomical regions. Five bones come together to create the floor of the cranial cavity through which vital nerves and blood vessels pass. This close proximity and its deep positioning make skull base surgery one of the most challenging areas of neurosurgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Despite its complexity, today there is no part of the skull base that is inaccessible and virtually no pathology that is inoperable,” says Badih Adada, MD, Chair of the Neurological Institute at Cleveland Clinic Florida and Chair of the Department of Neurosurgery. “Technology has driven a number of advancements as has the improved anatomical understanding of the brain and skull base.”
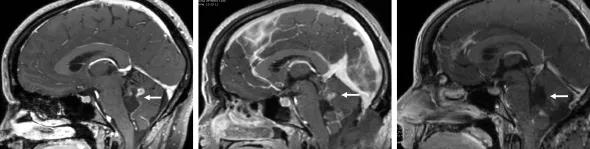
According to the National Brain Tumor Society, nearly 89,000 primary brain tumors will be diagnosed this year, of which there are more than 100 distinct types. Benign meningiomas are the most common and account for 39% of all primary brain tumors. Approximately 20-30% of these meningiomas occur in the skull base where arachnoid cap cells – the originator cells for meningiomas – are most abundant. Other types of skull base tumors include pituitary adenomas, craniopharyngiomas, which develop near the pituitary gland, and schwannoma, a type of nerve sheath tumor.
“Even though over two-thirds of brain tumors are benign, they can still cause significant harm as they grow by pressing upon the brain and nerves, and may require resection,” says Dr. Adada, who specializes in skull base and cerebrovascular surgery. He has performed more than 6,000 operations for complex brain tumors, aneurysms, epilepsy and spinal pathologies.
According to Dr. Adada, many skull base tumors can be removed using either an endoscopic approach or microscopic surgical techniques combined with small craniotomy. These less invasive procedures include endonasal endoscopic surgery, the supraorbital craniotomy, and the retromastoid craniotomy, among others.
Advertisement
“Determining the best approach for each individual patient entails identifying the shortest distance to the lesion and the greatest exposure that will allow for the safest resection,” explains Dr. Adada. “These minimally-invasive techniques are designed to maximize lesion resection while preserving neurological function. At Cleveland Clinic Florida, we do this with little to no brain retraction.”
Endonasal endoscopic surgery uses a natural corridor to manage skull base lesions, causing less tissue damage and a quicker recovery. This transnasal technique is used to access the sellar, medial and most of the lateral areas of the skull base. “For many years the cavernous sinus, located behind the eye sockets, was considered ‘no man’s land’ by neurosurgeons, but that is no longer the case,” Dr. Adada notes.
Advances in technology and instrumentation have supported the rapid development of these two surgical approaches, including the endoscope, operating microscope, and the more advanced 3D exoscope. Intraoperative neuronavigation using high-resolution MRI and CT imaging also allows for precise intraoperative localization and the avoidance of critical structures.
Detailed knowledge of skull base anatomy is needed to analyze pre-operative imaging studies and choose the most suitable approach as well as avoid complications. “These procedures also take exceptional technical skill and require a lot of practice to master,” adds Dr. Adada.
The Cleveland Clinic Florida Brain Tumor Center offers a clinical fellowship to train physicians in the subspecialties of open and endoscopic skull base surgery. It was established in 2019 and is one of 40 skull base surgery fellowships registered with the North American Skull Base Society.
Advertisement
During the fellowship year, the clinical fellow actively participates in ongoing clinical and lab research projects in collaboration with two research fellows. Clinical fellows also have 24/7 access to a state of the art anatomical lab on the Weston campus equipped with microscope and endoscope.
“As a high volume center for skull base surgery, our fellows gain plenty of hands on experience in addition to substantial lab-based training,” says Dr. Adada. “We are extremely pleased that Dr. Mauricio Mandel, our third fellow and the first to choose to practice in Florida, will be joining our neurosurgery team at Cleveland Clinic Tradition Hospital this summer.”
Cleveland Clinic uses a multidisciplinary team approach to care for patients with benign and malignant skull base tumors. Depending on the type and location of the lesion, the care team may include a neurosurgeon, an otolaryngologic surgeon, plastic surgeon, pituitary endocrinologist, neuroradiologist, medical oncologist and radiation oncologist.
In particular, endonasal procedures for skull base lesions require close collaboration between the neurosurgeon and ENT surgeon. “This simultaneous two-surgeon approach allows us to tackle a wide array of complex cranial base conditions, including endoscopic pituitary surgery,” says Dr. Adada.
Advertisement
Advertisement
Nonthermal technique reduces bleeding and perforation risk
Standardizing a minimally invasive approach for Barrett’s Esophagus and Esophageal Cancer
PSMA-targeted therapy for metastatic prostate cancer now offered at Cleveland Clinic Weston Hospital
Nationally recognized urologic oncologist offers vision for growth, innovation, and excellence
Noninvasive modality gains ground in United States for patients with early-to-moderate disease
Cleveland Clinic Weston Hospital’s collaborative model elevates care for complex lung diseases
Interventional pulmonologists at Cleveland Clinic Indian River Hospital use robotic technology to reach small peripheral lung nodules
Trained in the use of multiple focal therapies for prostate cancer, Dr. Jamil Syed recommends HIFU for certain patients with intermediate-risk prostate cancer, especially individuals with small, well-defined tumors localized to the lateral and posterior regions of the gland.