Approaching distal tibial nonunions
By Mark J. Berkowitz, MD, MBA and Damien Billow, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Nonunions of distal tibia fractures represent some of the most complex cases an orthopaedic surgeon can face. Distal tibial nonunions can be associated with open fracture, infection, poor skin quality, broken hardware and osteopenia. These factors, independently or in combination, can make successful reconstruction a challenge. For instance, in addition to the presence of traumatic lacerations, previous surgical incisions may have been placed in a suboptimal location, limiting the potential for alternative approaches. Similarly, broken hardware can interfere with the placement of new hardware needed during the revision procedure. Additionally, patient risk factors such as diabetes, smoking and peripheral vascular disease also contribute significantly to the incidence and complexity of nonunion in distal tibia fractures.
The status of the ankle joint itself can also further complicate reconstructive options. If the articular anatomy of the tibial plafond is in reasonable condition, then the focus of the reconstruction can be on addressing only the metaphyseal nonunion. However, if the damage to the plafond is severe enough that it is not deemed amenable to reconstruction, then a reconstructive procedure that combines ankle fusion with concomitant repair of the nonunion may need to be considered.
This article describes our preferred approach for addressing distal tibial nonunions, both when the ankle joint is spared as well as when the ankle cannot be salvaged and concomitant fusion is required.
Advertisement
Open distal tibia fractures with a medial laceration are often treated with an anterolateral plate to avoid placing hardware through the open wound. This construct may not be adequate to resist the significant bending and torsional forces in the distal leg, resulting in nonunion and breakage of the plate (Figure 1A, 1B). To address this complication, we have utilized a dual-plating technique along with aggressive cancellous bone graft that has been successful in achieving union of distal tibial metaphyseal nonunions.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/655bf580-4cdb-42c2-8887-9bf667a6a66c/19-ORT-1067-Leg-Repair-Fig-1_jpg)
Figure 1A, 1B: Anteroposterior (A) and lateral (B) radiographs demonstrate a distal tibial nonunion after medial open fracture initially treated with anterolateral plating. Note the fracture of the plate adjacent to the nonunion.
With this technique, careful attention must be paid to the handling of the skin and the placement of the surgical incisions. The previously placed anterolateral incision must be reopened to remove the broken hardware. A separate medial incision is required to fully expose the nonunion and to allow for biplanar plate fixation. The skin bridge between these two incisions must be maximized while minimizing undermining of the skin flaps to avoid marginal necrosis. A third posterolateral incision may be needed if the fibula also needs to be addressed.
Once hardware has been removed and the dual approach is exposed, the nonunion must be debrided to bleeding healthy bone. The resultant bone defect can be substantial and is filled with cancellous bone graft (Figure 2A, 2B). Both crushed allogenic bone mixed with bone marrow aspirate and retrograde femoral intramedullary cancellous autograft can be successful. Once the defect is densely packed, dual plate fixation is implanted consisting of a medial distal tibial locking plate and anterior T-plate. The medial plate allows for long-segment neutralization of varus/valgus forces while the anterior plate achieves fixation closer to the fracture site and in the plane of motion. This rigid biplanar construct has proven reproducible and effective in salvaging distal tibial nonunions when the ankle joint can be spared (Figure 3A, 3B).
Advertisement
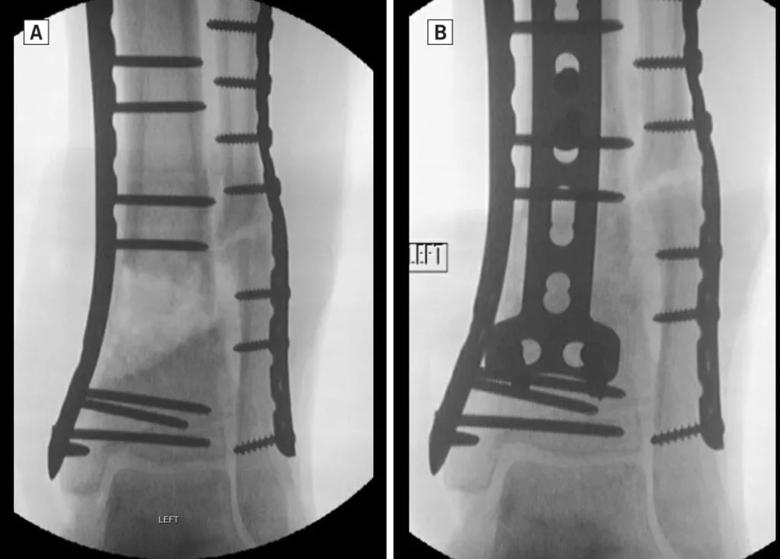
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/9cdd185f-5737-4d9d-a750-e23cb6f4e98f/19-ORT-1067-Leg-Repair-Fig-2-1024x734_jpg)
Figure 2A: Fluoroscopic anteroposterior (AP) image demonstrates the large metaphyseal bone defect present after debridement of the nonunion. Figure 2B: Fluoroscopic AP image demonstrates appearance after aggressive cancellous bone grafting using femoral intramedullary autograft. Note second anterior T-plate has been placed over the bone graft.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/46c5866a-fd87-4375-a47e-36ac96772040/19-ORT-1067-Leg-Repair-Fig-3_jpg)
Figure 3A, 3B: AP (A) and lateral (B) images demonstrate successful healing at six months of the distal tibia fracture nonunion in Figure 1 treated with double plating.
Unfortunately, intra-articular distal tibia fractures can, at times, damage the ankle joint surface so severely as to preclude reconstruction. In this instance, if nonunion develops, it may be necessary to consider fusion of the damaged ankle at the same time as reconstruction of the nonunion (Figure 4A, 4B). At Cleveland Clinic, we have found hindfoot nailing with limited plate and screw fixation of the nonunion to be an effective, albeit imperfect, approach to this problem. Although a hindfoot intramedullary nail provides rigid, low-profile, long-segment fixation of both the ankle fusion and the nonunion, it necessitates fusion of the subtalar joint as well with resultant hindfoot stiffness. This loss of hindfoot motion must be critically weighed against the putative benefits of this approach on a case-by-case basis to determine whether this approach is appropriate for a given patient.
With this technique, a transfibular approach is generally required for exposure of both the ankle and subtalar joints. An anteromedial incision is also usually needed to complete the ankle preparation and to fully expose and prepare the metaphyseal nonunion. Just as described previously, the nonunion must be aggressively debrided and packed with cancellous bone graft. Each of the major fracture fragments as well as the ankle joint itself are then pinned in appropriate alignment. Hindfoot nailing is then performed in standard fashion. Often compression is not needed or desirable due to the concomitant metaphyseal nonunion. However, one-third tubular plates and individual lag screws can be used to buttress and stabilize the major metaphyseal fragments, allowing for modest compression through the nail (Figure 5). Augmentation with bone morphogenetic protein is often indicated. The fibula can either be excised or preserved and stabilized with fixation screws (Figure 6).
Advertisement

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/9b6e23c5-0307-46ef-8382-00fb6087a251/19-ORT-1067-Leg-Repair-Fig-4_jpg)
Figure 4A, 4B: AP (A) and lateral (B) radiographs demonstrate distal tibia nonunion with severe disruption of the plafond joint surface.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/42ad221f-6704-4577-aec0-a04f9b22924d/19-ORT-1067-Leg-Repair-Fig-5_jpg)
Figure 5A, 5B: AP (A) and lateral (B) radiographs reveal successful reconstruction of the distal tibial nonunion and fusion of the ankle joint seven months after surgery. Note the one-third tubular plate and screws used to stabilize the major metaphyseal fracture fragments.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/95e34181-4d36-46f3-a89f-8d36994122d4/19-ORT-1067-Leg-Repair-Fig-6_jpg)
Figure 6 – AP fluoroscopic image from different patient reveals preservation of the distal fibula after osteotomy using screws for fixation.
Nonunion of a distal tibia fracture represents a severe and complex complication. Double plating with aggressive cancellous bone grafting is a viable technique for salvaging distal tibia metaphyseal nonunions. If the ankle joint is irreparably damaged as well, limited plating along with hindfoot nailing is a useful surgical option.
Dr. Berkowitz is an orthopaedic surgeon who specializes in Foot and Ankle Surgery and Lower Extremity Trauma. He is the Director of the Foot and Ankle Center within the Department of Orthopaedic Surgery at Cleveland Clinic.
Dr. Billow is an orthopaedic surgeon who specializes in Orthopaedic Traumatology. He is Director of the Orthopaedic Trauma Service at Cleveland Clinic.
Advertisement
Advertisement

How it’s similar but different from the direct anterior approach

Collaboration must cross borders and disciplines

Systematic review of MOON cohorts demonstrates a need for sex-specific rehab protocols

Should surgeons forgo posterior and lateral approaches?

How chiropractors can reduce unnecessary imaging, lower costs and ease the burden on primary care clinicians

Why shifting away from delayed repairs in high-risk athletes could prevent long-term instability and improve outcomes

Multidisciplinary care can make arthroplasty a safe option even for patients with low ejection fraction

Percutaneous stabilization can increase mobility without disrupting cancer treatment