Conventional arthroplasty performs better than reverse arthroplasty for patients with an intact rotator cuff
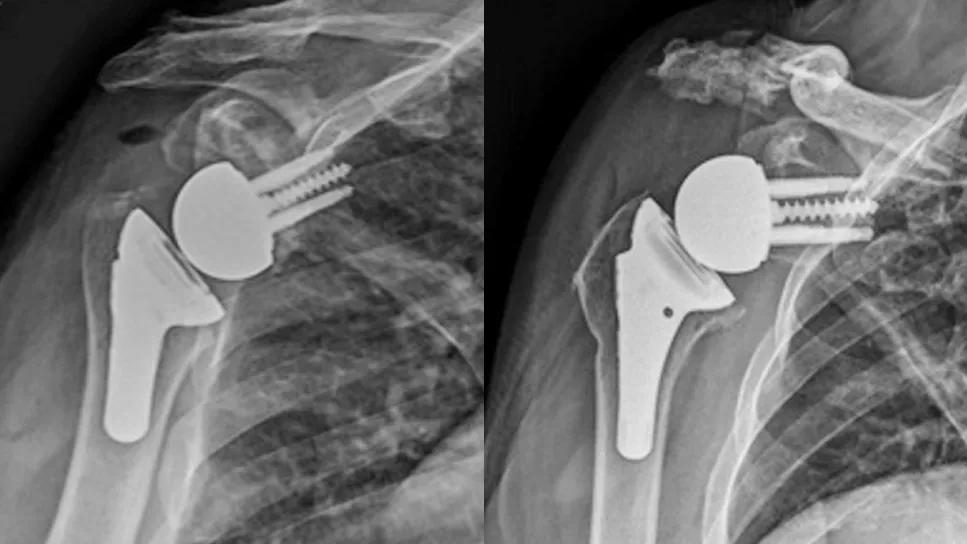
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/154e1104-6051-47bc-9765-8ef4b7f5d778/total-shoulder-replacement-feature2)
X-rays of total shoulder replacement
Conventional anatomic total shoulder arthroplasty (TSA) still has a place in patient care and should not be widely substituted with reverse TSA (rTSA), suggests a Cleveland Clinic study on patient-reported outcomes of shoulder replacement surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
As shoulder replacement surgery has evolved over the past four decades, rTSA has gone from a newer experimental technique to the most common type of shoulder replacement worldwide. Initially intended only for patients with rotator cuff tear arthropathy, rTSA now makes up approximately 70% of shoulder replacements in the U.S., including for patients with glenohumeral osteoarthritis.
“There’s been a lot of debate about whether reverse replacement is as good as anatomic replacement,” says Eric Ricchetti, MD, an orthopaedic surgeon specializing in shoulder surgery at Cleveland Clinic. “Some papers have shown that the procedures are basically equivalent, particularly for patients with intact rotator cuffs. However, these papers have studied relatively small groups of patients with less advanced statistical analysis.”
Enter Cleveland Clinic’s orthopaedic Outcomes Management and Evaluation (OME) database, which collects data from patients having elective shoulder, hip and knee surgeries. The database has collected nearly 100% of baseline data from Cleveland Clinic arthroplasty patients before surgery and approximately 70%-80% of patient-reported data at one-year follow-up, making the database a powerful tool for studying orthopaedic surgeries and their outcomes.
“Some orthopaedic surgeons argue that one implant type is generally better than the other, but it’s not that straightforward,” Dr. Ricchetti says. “There are many factors at play — factors that can overlap.”
To untangle the interaction of these factors, Dr. Ricchetti and colleagues studied the wealth of data in the OME database and published the most comprehensive study to date on short-term patient-reported outcomes of shoulder replacement surgery. According to the study published in the Journal of Shoulder and Elbow Surgery, the biggest driver of one-year outcomes of shoulder replacement surgery is a combination of diagnosis and implant type.
Advertisement
The researchers prospectively studied more than 1,000 (n = 1,042) patients who had primary shoulder replacement at Cleveland Clinic between 2015 and 2019:

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/94f530b8-334f-499a-a6a1-ba29f578e77b/total-shoulder-replacement-inset2)
Preoperative (top) and postoperative (bottom) X-rays of: a patient with glenohumeral osteoarthritis who underwent rTSA (A), a patient with rotator cuff tear arthropathy who underwent rTSA (B), and a patient with glenohumeral osteoarthritis who underwent anatomic TSA (C).
They reviewed the Penn Shoulder Scores (pain, function, satisfaction and total scores) reported by patients before and one year after surgery, and evaluated which patient, disease-specific and surgical factors most impacted the scores. The Penn Shoulder Score is a validated, shoulder-specific outcome tool using a scale of 0 to 100. Higher scores indicate better shoulder function, lower pain and higher satisfaction.
“Most research on this topic has assessed only a few predictive factors at a time, often in smaller cohorts of patients,” Dr. Ricchetti says. “We controlled for 20 predictive factors in over 1,000 patients and conducted a multivariable statistical analysis to rank factors in order of importance to outcome.”
Average Penn Shoulder Scores significantly improved one year after surgery for patients in all three treatment groups. However, certain preoperative factors were associated with lower scores, including younger age, female sex, current smoking, chronic pain diagnosis and history of prior surgery on the operative shoulder.
The factors that most strongly impacted Penn Shoulder Scores one year after surgery, ranked by importance, were:
Advertisement
“Patients who had anatomic TSA for glenohumeral osteoarthritis reported the highest Penn Shoulder Scores one year after surgery when controlling for a large number of other patient, disease and surgical factors — higher than the other categories of patients, including those who had rTSA for glenohumeral osteoarthritis,” Dr. Ricchetti says.
In addition, the study further supports that patients with rotator cuff tear arthropathy report worse outcomes after shoulder replacement surgery. It’s known in medical literature that patients with rotator cuff tears have slightly worse outcomes after rTSA, likely because they don’t have the same strength and function as patients with intact rotator cuffs. The data from Cleveland Clinic’s OME database affirmed this finding in the largest cohort to date.
When focusing on patients with glenohumeral osteoarthritis and intact rotator cuffs, medical literature hasn’t clearly shown that one type of TSA is better than another. The complex analysis by Dr. Ricchetti and colleagues is the first to reveal that anatomic TSA performs better than rTSA for these patients.
“The conventional anatomic replacement puts the implant in the normal position of the joint,” Dr. Ricchetti says. “The reverse replacement switches the position of the ball and socket, so the movement may not be as natural as with a conventional replacement. In particular, the published literature shows that patients with reverse shoulder replacements have less internal rotation motion than patients with conventional replacements. The more natural motion after a conventional replacement may be why patients are more satisfied with their shoulder after that procedure.”
Advertisement
Reverse TSAs, which have boomed in popularity in the past decade, may be the best option for some patients — particularly those with rotator cuff tears or those with more severe glenoid bone loss — but not for all.
“Conventional TSAs still can provide optimal outcomes,” Dr. Ricchetti says. “We should think twice about performing rTSAs in every patient and indicate patients based on the status of their rotator cuff and severity of bone loss. Reverse TSAs may not be preferable for all patients with intact rotator cuffs.”
Consider the right implant for each diagnosis, he says.
Based on this study, the research team developed an online tool to help predict Penn Shoulder Scores one year after primary TSA. To use this tool during presurgical counseling with your patients, see https://riskcalc.org/Predicting1YearPROMSAfterTotalShoulderArthroplasty.
Advertisement
Advertisement
Why shifting away from delayed repairs in high-risk athletes could prevent long-term instability and improve outcomes
Sinus tracts can occur years later and not near the incision site
Iliac crest structural autograft repairs large, uncontained defect
How it’s similar but different from the direct anterior approach
Collaboration must cross borders and disciplines
Systematic review of MOON cohorts demonstrates a need for sex-specific rehab protocols
Should surgeons forgo posterior and lateral approaches?
How chiropractors can reduce unnecessary imaging, lower costs and ease the burden on primary care clinicians