ESD should be considered to manage higher risk polyps
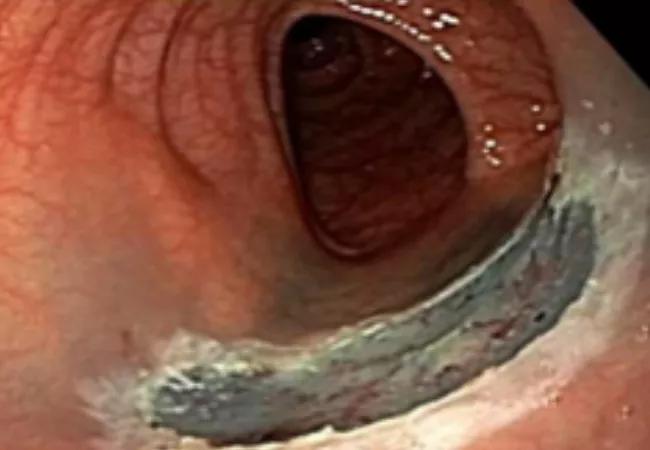
With the increase in screening colonoscopy programs in the United States and Europe, more large flat colon polyps are being detected. The need to remove these benign polyps is not questioned but the best way to resect them is controversial. In western countries, the standard of care is endoscopic mucosal resection (EMR) while in Japan and other Asian countries endoscopic submucosal dissection (ESD) has become the standard, as it allows for removal of the polyp in one complete piece and is associated with significantly lower polyp recurrence rates.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
There is resistance to the adoption of ESD in the West because it is more technically challenging to perform and most recurrences after piecemeal EMR are believed to be benign and treatable with repeat EMR.
Some patients who have large polyps with high-grade dysplasia removed by piecemeal resection develop invasive colorectal carcinoma (CRC) at the polypectomy site. “This is a terrible outcome and one we have to do our best to avoid,” says Cleveland Clinic gastroenterologist Amit Bhatt, MD.
To learn more about the incidence and risk factors for local polyp recurrence following endoscopic removal, Dr. Bhatt and a team from the Department of Gastroenterology, Hepatology and Nutrition conducted a retrospective study of 229 patients with large colon polyps with high-grade dysplasia that were completely resected at Cleveland Clinic from 2000 to 2016. A total of 254 lesions (median size 29.2 mm) were resected, 138 by piecemeal and 116 en-bloc.
Cancer was diagnosed at the site of polypectomy on follow-up in six cases. Of these six cases, three cases were diagnosed at an early stage (I or II) and three cases were diagnosed at an advanced stage (III or IV). In three cases, the location was ascending and cecum and the remaining three were sigmoid, descending and transverse. The median time to cancer diagnosis was 28.5 months. Distant metastatic disease was found at the time of diagnosis in two cases. Based on time-to-event analysis, the estimated incidence of cancer related to the index polyp was 1.3 percent at one year and 4.5 percent at five years.
Advertisement
“While recurrence with malignancy is a rare event, it is a major one with serious implications for patients. These findings tip the balance towards ESD, and away from EMR for the removal of higher risk colon polyps. Taking the time to make sure these high-risk polyps are completely removed with ESD makes sense,” says Dr. Bhatt, senior author of the study. The first author of the study is Ashraf Abushahin, MD, an internal medicine resident at Cleveland Clinic, who helped execute and write the study.
All of the malignant cases occurred after piecemeal resection and none after en-bloc resection. “When a polyp is removed in multiple pieces by piecemeal EMR, it is hard to make sure that the entire polyp is removed, and it is difficult for the pathologist to give precise histopathologic information on the polyp,” says Dr. Bhatt. “When a polyp is removed by en-bloc resection by ESD, you can perform a more precise histological analysis that lets us know if the polyp is completely removed and if any high risk features are present.”
Based on this evidence “patients with large polyps with high-grade dysplasia should have close endoscopic surveillance and be offered the option of ESD en-bloc resection. This technique takes more time and fewer doctors are trained to perform it; there is always apprehension about changing standard procedures and learning something new,” says Dr. Bhatt.
“However, this study helps make the argument for ESD en-bloc resection of high-risk polyps. It shows that with a select patient population, this type of resection may be truly beneficial and worth the extra effort.”
Advertisement
The study was presented today at the American Congress of Gastroenterology (ACG) annual meeting.
Advertisement
Advertisement

Benefits of neoadjuvant immunotherapy reflect emerging standard of care

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Potentially cost-effective addition to standard GERD management in post-transplant patients

Findings could help clinicians make more informed decisions about medication recommendations

Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care

Retrospective analysis looks at data from more than 5000 patients across 40 years