The disease is not a barrier to pregnancy, but risks from disease-modifying therapies must be managed

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b4e893eb-3aad-4431-a284-6407e278ad97/fertility-preservation-in-young-adults-cancer-2084337795)
Baby feet
By Alise Carlson, MD; Daniel Ontaneda, MD, PhD; Mary Rensel, MD; Jeffrey Cohen, MD; and Amy Kunchok, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Note: This article is republished from the Cleveland Clinic Journal of Medicine (2023;90[4]:235-243). The original can be found here.
Multiple sclerosis (MS), a chronic, inflammatory, neurodegenerative disease, is often diagnosed during patients’ childbearing years. As a result, family planning, contraception, pregnancy and childbirth are significant concerns. Healthcare for people with MS requires access to information and clinicians who can provide guidance. MS itself is not a barrier to pregnancy, but disease-modifying therapies (DMTs) for MS are associated with varying degrees of risks to the fetus. Many risks are theoretical due to limited fetal safety data, but they require careful consideration by both clinician and patient.
Clinicians at the Cleveland Clinic Mellen Center for Multiple Sclerosis developed a collaborative approach to reproductive health and MS, a summary of which is available on the Mellen Center website.1 This article, based on the Mellen Center consensus initiative, combines a review of the literature with clinical experience to address 20 frequently asked questions about the management of MS during family planning, pregnancy and the postpartum period.
Sexual dysfunction affects 40% to 80% of women and 50% to 90% of men who have MS,2 imposing a significant negative impact on quality of life. Targeted symptomatic therapies such as lubricants, sex steroid therapy, prostaglandins, phosphodiesterase 5 inhibitors or psychotherapy may be used. When symptomatic therapies are unsuccessful, patients may benefit from further evaluation by gynecologic or urologic specialists.3
Advertisement
Conception and fertility rates in people with MS and the general population are comparable. The use of assisted reproductive technology has been reported in some studies to be associated with an increased risk of MS relapse in the first three months following unsuccessful cycles.4 However, a recently published study did not identify this risk.5
Children of people with MS are approximately 5.77 times more likely to develop MS than people in the general population,6 though the overall risk remains low at approximately 2%.7 Although genetic factors contribute to susceptibility to MS, the disorder is complex, with more than 250 identified contributory genes. The development of MS likely also depends on environmental and other factors, including exposure to smoking, viral infections, adolescent obesity, vitamin D levels, microbiome and geographic latitude of residence.8
The choice of DMT should be based on the patient’s level of disease activity, their plans to become pregnant and the desired timing. Most DMTs are associated with fetal risk; further, the sphingosine 1-phosphate receptor (S1Pr) modulators and natalizumab are associated with a risk of rebound disease activity upon discontinuation.
Women with MS of childbearing potential who are using DMT should practice effective birth control regardless of plans to pursue pregnancy. In general, contraceptive methods used in the population at large are safe and effective for women with MS. Potential drug-drug interactions between symptomatic treatments (for MS-related sequelae such as spasticity, urinary dysfunction and mood dysregulation) and certain contraceptive agents should be considered: for example, modafinil may lessen the efficacy of oral contraceptives by accelerating their metabolism.
Advertisement
Men with MS treated with teriflunomide, which carries significant risk of teratogenicity, must practice effective contraception until after the medication is cleared by metabolism (i.e., at least six months after the last dose) or by a rapid-clearance protocol. Female partners of men taking teriflunomide must also be counseled on the potential risks of fetal exposure and the use of effective contraceptive therapy. Teriflunomide is contraindicated for use during pregnancy and in females of reproductive age not using effective contraception.
Cladribine has been associated with increased embryo lethality in animal studies, and men are thus advised to prevent pregnancy for at least six months following treatment with cladribine.9 Cladribine may cause an increase in nonmotile sperm, leading to reversible infertility.10
Alemtuzumab may cause reversible infertility by inactivating mature sperm by binding to CD52, the surface antigen expressed by mature sperm.11
MS itself does not render a pregnancy “high risk” or increase the likelihood of congenital malformation or miscarriage. MS may be associated with lower birthweight,4 although this is usually not clinically significant.
The overall risk of MS relapse decreases during pregnancy, with the relapse rate declining progressively over the three trimesters.12 The patient’s recent disease trajectory and her prior DMT pharmacology, efficacy and latency may influence disease activity during pregnancy. Women with higher relapse rates prior to conception are at increased risk of ongoing disease activity during pregnancy.12
Advertisement
The use of DMT is generally not recommended during pregnancy. Treatment considerations must include the potential benefits and risks to the mother based on her level of disease activity and the likelihood of relapse or worsening disability without DMT. Embryonic or fetal exposure is also associated with risk (Table 1).1,5,10,11,13–41
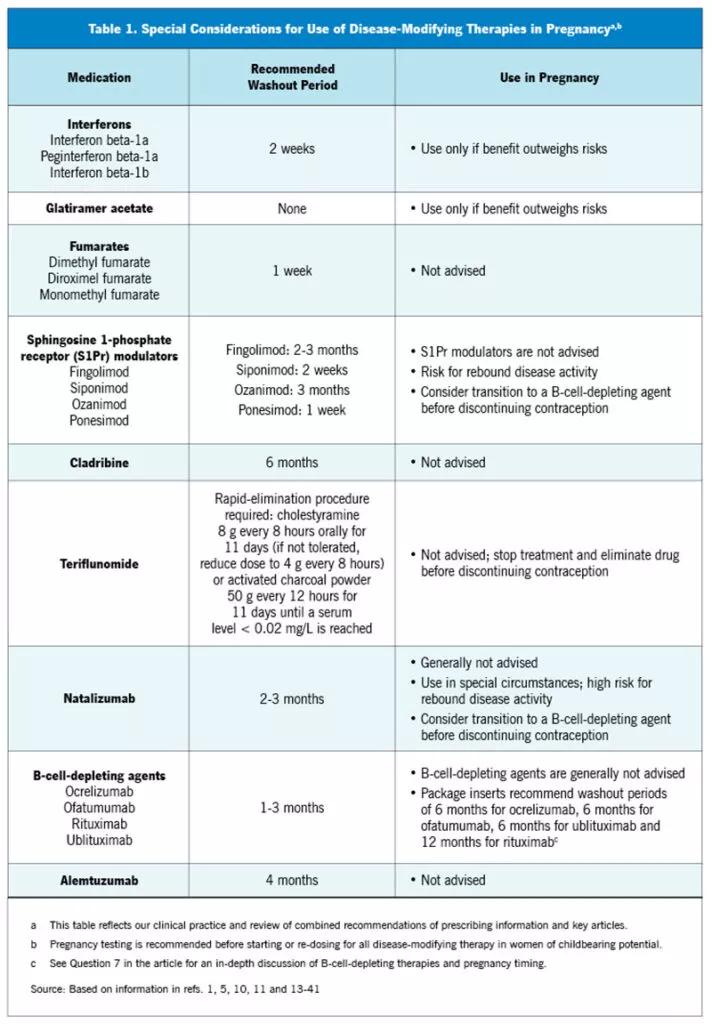
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c0d89b52-8504-46cb-bdc3-002f5770f19c/23-NEU-4060108-CQD-Inset-First-Table-800x1150-1-712x1024_jpg)
Special considerations for using disease-modifying therapies in pregnancy
Platform injectable therapies. The first DMTs — the “platform therapies,” i.e., interferons13–17 and glatiramer acetate18,19 — have been associated with low birthweight but not with other significant adverse effects on pregnancy. These treatments are generally stopped before planned conception. However, when benefits outweigh risks, they may be continued in women with MS who are pregnant or wish to become pregnant and whose risk profile is low.
Monoclonal antibodies. With few exceptions, the use of monoclonal antibodies during pregnancy is not advised. Placental transfer of immunoglobulins begins around the second trimester and increases with gestational age, theoretically lowering the risk of fetal exposure in the first trimester.20 Natalizumab may be considered during pregnancy in exceptional circumstances, as in women with severe intrapartum relapses.12 Its use during the third trimester requires caution because of risk of placental transfer and resulting fetal or infantile pancytopenia.21 B-cell-depleting therapies (ocrelizumab, ofatumumab, rituximab, ublituximab)22–26 can be used prior to pregnancy, but their routine administration is not recommended during pregnancy. Use of alemtuzumab during pregnancy is not advised.27
Advertisement
Oral therapies. None of the currently available oral therapies — fumarates,28–30 teriflunomide,31 S1Pr modulators32–35 or cladribine10 — are safe for use during pregnancy.
Washout periods are advised for all DMTs, with consideration of the pharmacokinetics of each medication and the patient’s level of disease activity. The pharmacology of the treatment determines recommended minimum washout periods (Table 1). When feasible, the timing of treatment and conception should be coordinated with the aim of keeping DMT washout periods as short as possible to mitigate risk of MS relapse.
Prescribing information approved by the FDA recommends that women continue contraception for six months following the last treatment with ocrelizumab,22 ofatumumab23 and ublituximab26 and for 12 months following the last treatment with rituximab.24,25 A pregnancy test should be conducted before subsequent dosing of intravenous B-cell-depleting therapies. Ofatumumab is administered by monthly subcutaneous injection, and the FDA-approved prescribing information recommends contraception for six months following the last treatment.23 Ofatumumab is thought to protect against disease activity for six to nine months.23
B-cell-depleting therapies infused intravenously may confer prolonged protective effects against MS relapses for six to nine months after administration. Decisions regarding use of B-cell-depleting therapy and pregnancy planning need to consider the patient’s degree of disease activity, risks and individual preferences. When disease is highly active before initiation of B-cell-depleting therapy and it is necessary to minimize time off DMT, the patient may receive a B-cell-depleting therapy and then attempt pregnancy after one to three months.36,42,43 The rationale is that based on half-life, these therapies are eliminated 3.5 to 4.5 months after an infusion.22,24,25 Placental transfer of immunoglobulin G is minimal in the first trimester,20 so the risk of fetal exposure in the second trimester is low if conception occurs three to six months after the last dose of B-cell-depleting therapy.36
Women treated with S1Pr modulators or natalizumab before conception may have increased risk for rebound disease after medication withdrawal. Annualized MS relapse rates have been shown to be higher throughout pregnancy after fingolimod and natalizumab discontinuation compared with low-efficacy therapies.12 In women discontinuing natalizumab, relapses during pregnancy and the postpartum year have been reported in up to 67% of patients.37 Due to the risk of rebound disease activity in people with MS treated with these medications, changing to an alternate therapy, such as a B-cell-depleting agent, might be considered before discontinuing contraception, especially in women with highly active disease.44
If a patient becomes pregnant while taking DMT, the therapy should be discontinued and the pregnancy exposure reported through an appropriate MS pregnancy registry (Table 2).1,5,10,11,13–41 Follow-up after discontinuation of therapy varies depending on the DMT, as follows:
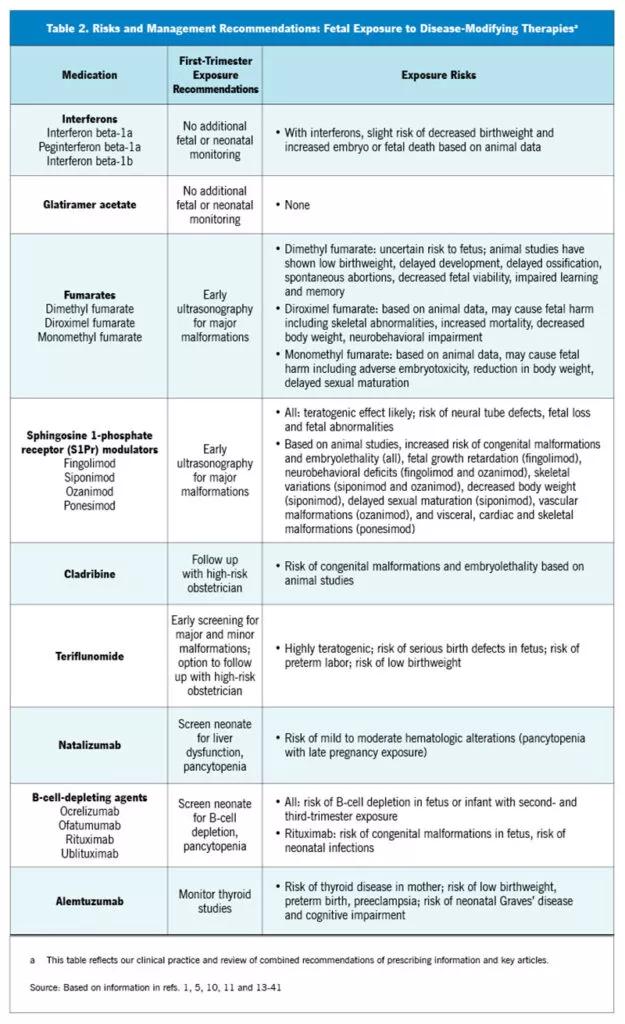
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/42a6728a-e7d4-44e8-ab84-68ce0d3a1100/23-NEU-4060108-CQD-Inset-Second-Table-800x1310-1-625x1024_jpg)
The patient’s obstetrician and neurologist should coordinate management of MS relapses during pregnancy. Mild relapses with nondisabling symptoms or spontaneous improvement might require no intervention. If a relapse warrants intervention, the typical treatment is high-dose corticosteroids, usually intravenous methylprednisolone 1 g daily or oral prednisone 1,250 mg daily for three to five days. This therapy carries a slightly increased risk for adverse fetal outcomes such as cleft palate and low birthweight.36 Maternal risks include hyperglycemia, hypertension and fluid overload.
Corticosteroid use should be avoided during the first trimester when possible. If the patient develops a disabling steroid-refractory relapse, then intravenous immunoglobulin therapy45 or plasmapheresis may be considered. The increased thrombotic risk with intravenous immunoglobulin should be taken into consideration. Nonpharmacologic interventions such as physical therapy can be used when deemed appropriate by the patient’s care team.
Despite there being no absolute contraindications to MRI during pregnancy, it is generally avoided. It can be done if clinically indicated, as when findings are critical to clinical decision-making and are expected to impact outcomes. Gadolinium-based contrast should be used with caution, as studies have associated it with increased risk of stillbirth, neonatal death and various inflammatory conditions.46
Barring contraindications, the vaccination schedule for the general population is applicable to people with MS.47 Vaccination updates are best before starting DMT. Any live attenuated vaccines that need to be updated may be administered following delivery and before restarting DMT.
For most women, there are no MS-specific recommendations for childbirth. Many women can have spontaneous-onset labor and full-term vaginal delivery. Individual factors may need to be considered for women with significant disability, such as planning for assisted delivery methods or cesarean delivery in women with significant motor disability, increased risk of deep vein thrombosis in nonambulatory patients, and increased risk of urinary tract infection in women requiring self-catheterization. The use of any anesthetic is acceptable when clinically indicated,48 including regional anesthesia as with epidural injections.
Neurologic care generally should resume four to six weeks postpartum. At that time, breastfeeding plans should be confirmed or revised and resumption of DMT arranged. Women with MS should receive routine obstetric postpartum care, and duration of birth hospitalizations are in the normal range.49 Patients should be screened for depression and anxiety at follow-up visits. The risk of perinatal depression is higher than in the general population, although the prognosis for recovery at 18 months is similar.50
Women with MS may be at risk for return of disease activity in the postpartum period. Higher relapse rates before pregnancy are associated with higher postpartum relapse rates. Approximately 13% of women with term or preterm deliveries experience a clinical relapse within three months of delivery.12
Breastfeeding plans and timing of DMT resumption should be discussed prior to delivery. When to resume DMT is an individual decision that needs to account for previous disease activity and breastfeeding plans. Resumption of DMT early postpartum should be considered for women with highly active disease before conception or relapse during pregnancy. Women with a low level of disease activity may reasonably defer DMT resumption while they are breastfeeding.
Data are limited concerning the safety of DMT for the breastfed infant, so use of DMT during breastfeeding is generally not advised. The decision to breastfeed and its duration should balance its benefits with the risk of relapse. Notably, the decision to breastfeed requires a delay in DMT resumption that may increase the risk of relapse. The patient’s disease characteristics must be considered.
Most DMTs are considered unsafe for use during breastfeeding. The exception is glatiramer acetate, recently approved by European Union health authorities for use during breastfeeding38 based on the rationale that benefits of breastfeeding likely exceed the risk of exposure.
The degree of transfer of DMTs into breast milk depends on the size of the molecule. Interferon beta molecules are larger than 20kDa, and glatiramer acetate molecules are 5 to 9 kDa, and the amount of transfer to breast milk is low.51 B-cell-depleting therapies involve much larger molecules, on the scale of 145 kDa, and their low oral bioavailability limits absorption by the newborn; the relative infant dose is less than 10%.39 Even so, B-cell-depleting therapies may have clinical implications for the infant such as B-cell depletion and impaired vaccine responses, though this concern remains theoretical.
Natalizumab is detectable in breast milk in small amounts and therefore should also be used with caution.51 Dimethyl fumarate, S1Pr modulators, cladribine, alemtuzumab and teriflunomide should not be used during breastfeeding in view of their risk profiles (Table 2).36,40
Relapses of MS that occur during breastfeeding can be treated as they usually would be. Transfer of methylprednisolone through breastmilk is thought to be minimal and may be further minimized by delaying breastfeeding for two to four hours after treatment, as levels peak approximately two hours after infusion and decline rapidly thereafter, falling below the limits of detection 24 hours after infusion.52,53 For women receiving oral prednisone, the dose ingested by the infant through breastmilk is thought to be negligible, and no adverse effects have been reported in infants breastfed by mothers in general receiving oral corticosteroid treatment.41
Gadolinium contrast for MRI studies may be used while breastfeeding when clinically necessary; although small amounts are detectable in breastmilk, there is little gastrointestinal absorption.54 If there is any concern for potential toxicity, the patient may refrain from breastfeeding or discard breastmilk for 12 to 24 hours after contrast administration.
Infertility is common in both men and women after autologous hematopoietic stem cell transplant, and gonadal toxicity results from the cytotoxic therapies that make up the mobilization and conditioning regimens.55 Therefore, pretreatment counseling regarding the risk of infertility is critical. People with MS may wish to consider fertility preservation such as cryopreservation of sperm, mature oocytes or fertilized embryos, and referral to an oncofertility specialist may be appropriate. Limited data suggest that infants born to women who have undergone autologous hematopoietic stem cell transplant do not have an increased risk of congenital abnormalities.55
Management of MS is complex and requires individualized treatment, and pregnancy and reproductive issues are often at the forefront of concerns for both women and men of reproductive age. The individual’s care team, including the primary care clinician, internist, obstetrician and neurologist, need to engage in collaborative decision-making before, during and after pregnancy to optimize the management of MS-related reproductive issues.
1. Cleveland Clinic Mellen Center for Multiple Sclerosis. Mellen Center approach: management of multiple sclerosis during pregnancy. Updated October 14, 2021. https://my.clevelandclinic.org/-/scassets/files/org/neurological/mellen-center/management-of-multiple-sclerosis-during-pregnancy.pdf. Accessed March 13, 2023.
2. Drulovic J, Kisic-Tepavcevic D, Pekmezovic T. Epidemiology, diagnosis and management of sexual dysfunction in multiple sclerosis. Acta Neurol Belg. 2020;120(4):791-797.
3. Guo ZN, He SY, Zhang HL, Wu J, Yang Y. Multiple sclerosis and sexual dysfunction. Asian J Androl. 2012;14(4):530-535.
4. Hellwig K. Pregnancy in multiple sclerosis. Eur Neurol. 2014;72(suppl 1):39-42.
5. Mainguy M, Tillaut H, Degremont A, et al. Assessing the risk of relapse requiring corticosteroids after in vitro fertilization in women with multiple sclerosis. Neurology. 2022; 10.1212/WNL.0000000000201027.
6. Westerlind H, Ramanujam R, Uvehag D, et al. Modest familial risks for multiple sclerosis: a registry-based study of the population of Sweden. Brain. 2014;137(Pt 3):770-778.
7. Balcerac A, Louapre C. Genetics and familial distribution of multiple sclerosis: A review. Rev Neurol (Paris). 2022;178(6):512-520.
8. Simpson S Jr., Blizzard L, Otahal P, Van der Mei I, Taylor B. Latitude is significantly associated with the prevalence of multiple sclerosis: a meta-analysis. J Neurol Neurosurg Psychiatry. 2011;82(10):1132-1141.
9. Cook S, Vermersch P, Comi G, et al. Safety and tolerability of cladribine tablets in multiple sclerosis: the CLARITY (CLAdRIbine Tablets treating multiple sclerosis orallY) study. Mult Scler. 2011;17(5):578-593.
10. EMD Serono, Inc. Mavenclad (cladribine) package insert. https://www.emdserono.com/us-en/pi/mavenclad-pi.pdf. Accessed March 13, 2023.
11. Cree BA. Update on reproductive safety of current and emerging disease-modifying therapies for multiple sclerosis. Mult Scler. 2013;19(7):835-843.
12. Yeh WZ, Widyastuti PA, Van der Walt A, et al. Natalizumab, fingolimod and dimethyl fumarate use and pregnancy-related relapse and disability in women with multiple sclerosis. Neurology. 2021;96(24):e2989-e3002.
13. Bayer HealthCare Pharmaceuticals, Inc. Betaseron (interferon-1b) package insert. https://labeling.bayerhealthcare.com/html/products/pi/Betaseron_PI.pdf. Accessed March 13, 2023.
14. Biogen, Inc. Avonex (interferon beta-1a) package insert. https://www.avonex.com/content/dam/commercial/avonex/pat/en_us/pdf/Avonex_US_Prescribing_Information.pdf. Accessed March 13, 2023.
15. EMD Serono, Inc. Rebif (interferon beta-1a) package insert. https://www.emdserono.com/us-en/pi/rebif-pi.pdf. Accessed March 13, 2023.
16. Biogen, Inc. Plegridy (peginterferon beta-1a) package insert. https://www.plegridy.com/content/dam/commercial/plegridy/pat/en_us/pdf/plegridy-prescribing-information.pdf. Accessed March 13, 2023.
17. Novartis Pharmaceuticals Corp. Extavia (interferon-1b) package insert. https://www.novartis.com/us-en/sites/novartis_us/files/extavia.pdf. Accessed March 13, 2023.
18. Teva Neuroscience, Inc. Copaxone (glatiramer acetate) package insert. https://www.copaxone.com/globalassets/copaxone/prescribing-information.pdf. Accessed March 13, 2023.
19. Sandoz, Inc. Glatopa (glatiramer acetate) package insert. https://www.glatopa.com/globalassets/glatopa-com/pdf/glatopa20_40_pi_2018.pdf. Accessed March 13, 2023.
20. DeSesso JM, Williams AL, Ahuja A, Bowman CJ, Hurtt ME. The placenta, transfer of immunoglobulins, and safety assessment of biopharmaceuticals in pregnancy. Crit Rev Toxicol. 2012;42(3):185-210.
21. Biogen, Inc. Tysabri (natalizumab) package insert. https://www.tysa-bri.com/content/dam/commercial/tysabri/pat/en_us/pdf/tysabri_prescribing_information.pdf. Accessed March 13, 2023.
22. Genentech, Inc. Ocrevus (ocrelizumab) package insert. https://www.gene.com/download/pdf/ocrevus_prescribing.pdf. Accessed March 13, 2023.
23. Novartis Pharmaceuticals Corp. Kesimpta (ofatumumab) package insert. https://www.novartis.com/us-en/sites/novartis_us/files/kesimp-ta.pdf. Accessed March 13, 2023.
24. Genentech, Inc. Rituxan (rituximab) package insert. https://www.gene.com/download/pdf/rituxan_prescribing.pdf. Accessed March 13, 2023.
25. Pfizer. Ruxience (rituximab-pvrr) package insert. https://labeling.pfizer.com/ShowLabeling.aspx?id=12090. Accessed March 8, 2023.
26. TG Therapeutics. Briumvi (ublituximab-xiiy) package insert. https://www.tgtherapeutics.com/label-prescribing-info/uspi-briumvi.pdf. Accessed March 13, 2023.
27. Genzyme Corp. Lemtrada (alemtuzumab) package insert. https://products.sanofi.us/lemtrada/lemtrada.pdf. Accessed March 8, 2023.
28. Biogen, Inc. Tecfidera (dimethyl fumarate) package insert. https://www.tecfidera.com/content/dam/commercial/tecfidera/pat/en_us/pdf/full-prescribing-info.pdf. Accessed March 13, 2023.
29. Biogen, Inc. Vumerity (diroximel fumarate) package insert. https://www.vumerity.com/content/dam/commercial/vumerity/pat/en_us/pdf/vumerity-prescribing-information.pdf. Accessed March 13, 2023.
30. Banner Life Sciences, LLC. Bafiertam (monomethyl fumarate) package insert. https://www.bafiertam.com/pdf/bafiertam-prescribing-information.pdf. Accessed March 13, 2023.
31. Genzyme Corp. Aubagio (teriflunomide) package insert. https://products.sanofi.us/aubagio/aubagio.pdf. Accessed March 13, 2023.
32. Novartis Pharmaceuticals Corp. Gilenya (fingolimod) package insert https://www.novartis.com/us-en/sites/novartis_us/files/gilenya.pdf. Accessed March 13, 2023.
33. Novartis Pharmaceuticals Corp. Mayzent (siponimod) package insert. https://www.novartis.com/us-en/sites/novartis_us/files/mayzent.pdf. Accessed March 13, 2023.
34. Bristol Meyers Squibb. Zeposia (ozanimod) package insert. https://pack-ageinserts.bms.com/pi/pi_zeposia.pdf. Accessed March 13, 2023.
35. Janssen Pharmaceuticals, Inc. Ponvory (ponesimod) package insert. https://www.janssenlabels.com/package-insert/product-monograph/prescribing-information/PONVORY-pi.pdf. Accessed March 13, 2023.
36. Langer-Gould AM. Pregnancy and family planning in multiple sclerosis. Continuum (Minneap Minn). 2019;25(3):773-792.
37. Hellwig K, Tokic M, Thiel S, et al. Multiple sclerosis disease activity and disability following discontinuation of natalizumab for pregnancy. JAMA Netw Open. 2022;5(1):e2144750.
38. Ciplea AI, Kurzeja A, Thiel S, et al. Eighteen-month safety analysis of offspring breastfed by mothers receiving glatiramer acetate therapy for relapsing multiple sclerosis — COBRA study. Mult Scler. 2022;28(10):1641-1650.
39. Bove RM, Houtchens MK. Pregnancy management in multiple sclerosis and other demyelinating diseases. Continuum (Minneap Minn). 2022;28(1):12-33.
40. Krysko KM, LaHue SC, Anderson A, et al. Minimal breast milk transfer of rituximab, a monoclonal antibody used in neurological conditions. Neurol Neuroimmunol Neuroinflamm. 2019;7(1):e637.
41. National Library of Medicine. Prednisone. In: Drugs and Lactation Database (LactMed). Bethesda, MD: National Library of Medicine; 2021.
42. Langer-Gould A, Smith J, Albers K, et al. Pregnancy-related relapses in a large, contemporary multiple sclerosis cohort: no increased risk in the postpartum period. Presented at: American Academy of Neurology Annual Meeting; May 4-9, 2019; Philadelphia, PA.
43. Krysko KM, Bove R, Dobson R, Jokubaitis V, Hellwig K. Treatment of women with multiple sclerosis planning pregnancy. Curr Treat Options Neurol. 2021;23(4):11.
44. Alping P, Frisell T, Novakova L, et al. Rituximab versus fingolimod after natalizumab in multiple sclerosis patients. Ann Neurol. 2016;79(6):950-958.
45. Winkelmann A, Rommer PS, Hecker M, Zettl UK. Intravenous immunoglobulin treatment in multiple sclerosis: a prospective, rater-blinded analysis of relapse rates during pregnancy and the postnatal period. CNS Neurosci Ther. 2019;25(1):78-85.
46. Ray JG, Vermeulen MJ, Bharatha A, Montanera WJ, Park AL. Association between MRI exposure during pregnancy and fetal and childhood outcomes. JAMA. 2016; 316(9):952-961.
47. US Centers for Disease Control and Prevention. Guidelines for vaccinating pregnant women. Updated July 13, 2022. https://www.cdc.gov/vaccines/pregnancy/hcp-toolkit/guidelines.html. Accessed March 13, 2023.
48. Pastò L, Portaccio E, Ghezzi A, et al. Epidural analgesia and cesarean delivery in multiple sclerosis post-partum relapses: the Italian cohort study. BMC Neurol. 2012;12:165.
49. Lu E, Zhao Y, Dahlgren L, et al. Obstetrical epidural and spinal anesthesia in multiple sclerosis. J Neurol. 2013;260(10):2620-2628.
50. Eid K, Torkildsen ØF, Aarseth J, et al. Perinatal depression and anxiety in women with multiple sclerosis: a population-based cohort study. Neurology. 2021;96(23):e2789-e2800.
51. Fragoso YD, Adoni T, Alves-Leon SV, et al. Postpartum treatment with immunoglobulin does not prevent relapses of multiple sclerosis in the mother. Health Care Women Int. 2015;36(10):1072-1080.
52. Boz C, Terzi M, Zengin Karahan S, Sen S, Sarac Y, Emrah Mavis M. Safety of IV pulse methylprednisolone therapy during breastfeeding in patients with multiple sclerosis. Mult Scler. 2018;24(9):1205-1211.
53. Zengin Karahan S, Boz C, Terzi M, et al. Methylprednisolone concentrations in breast milk and serum of patients with multiple sclerosis treated with IV pulse methylprednisolone. Clin Neurol Neurosurg. 2020;197:106118.
54. ACR Committee on Drugs and Contrast Media. ACR Manual on Contrast Media: 2022. https://www.acr.org/-/media/ACR/files/clinical-resources/contrast_media.pdf. Accessed March 13, 2023.
55. Tichelli A, Rovó A. Fertility issues following hematopoietic stem cell transplantation. Expert Rev Hematol. 2013;6(4):375-388.
All authors are neurologists with Cleveland Clinic’s Mellen Center for Multiple Sclerosis.
Advertisement
Mixed results from phase 2 CALLIPER trial of novel dual-action compound
A co-author of the new recommendations shares the updates you need to know
Rebound risk is shaped by patient characteristics and mechanism of action of current DMT
First-of-kind prediction model demonstrates high consistency across internal and external validation
Real-world study also finds no significant rise in ocrelizumab-related risk with advanced age
Machine learning study associates discrete neuropsychological testing profiles with neurodegeneration
This MRI marker of inflammation can help differentiate MS from mimics early in the disease
Focuses include real-world research, expanding access and more