Caution warranted when prescribing antibiotics to these patients
Antibiotic therapy is associated with decreased time to cancer recurrence and survival in women with advanced epithelial ovarian cancer (EOC) being treated with platinum chemotherapy, according to a new study from Cleveland Clinic.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Studies in non-gynecologic cancers have demonstrated that antibiotics may negatively affect treatment outcomes. Since response to platinum chemotherapy is the biggest predictor of survival for women with EOC, identifying factors that lead to resistance is essential to improving survival. It is important for us to know if doing something we think is helping, like prescribing antibiotics, could hurt a patient’s chances of survival by making them more resistant to treatment,” says Laura Chambers, DO. “That’s exactly what we found.”
While this finding highlights an association, antibiotics may lead to or promote resistance to platinum chemotherapy, which is considered standard treatment for women with EOC.
In this retrospective study, which was recently published in Gynecologic Oncology, researchers looked at 424 women with newly diagnosed stage III or IV EOC who underwent cytoreductive surgery and then PC from 2009 and 2015. Of that group, 147 women received antibiotic treatment, and 48 received antibiotic treatment against gram-positive bacteria, for at least 48 hours.
These patients were given antibiotics for a variety of reasons, including neutropenic sepsis, urinary tract infections, pneumonia/upper-respiratory infections, cellulitis, gastrointestinal infections, neutropenic fever and bacteremia.
Researchers found that women who received antibiotics had worse outcomes compared with those who did not. Of patients who received antibiotics during chemotherapy, 86.4% had a recurrence of their cancer compared with 73.6% in patients who did not receive antibiotics. Outcomes are worse for those who had antibiotic treatment specifically targeting a type of bacteria, namely gram-positive bacteria: 93.8% had a recurrence. Antibiotic use was associated with a significant reduction in progression-free and overall survival.
Advertisement
And it’s not a small effect on overall survival. Patients who received antibiotics lived 45.6 months versus 62.4 months for those who did not. Patients who received antibiotic treatment against gram positive bacteria lived only 35.0 months.
“There was a survival difference of approximately 17 months, which is a lot of time considering new drugs struggle to demonstrate any overall survival benefits,” adds Roberto Vargas, MD, clinical assistant professor at the Cleveland Clinic Lerner College of Medicine and Case Western Reserve University, and associate staff in Gynecologic Oncology at Cleveland Clinic. “If we are judicious with our antibiotic treatments, particularly during chemotherapy, we could potentially give the gift of time to patients and their families.”
Dr. Vargas says the magnitude of differences in overall survival rate and cancer recurrence rates were surprising. “I can’t remember the last study in which there was a survival difference of this magnitude,” he says. However, the fact that antibiotic use was associated with worse outcomes did not come as a surprise.
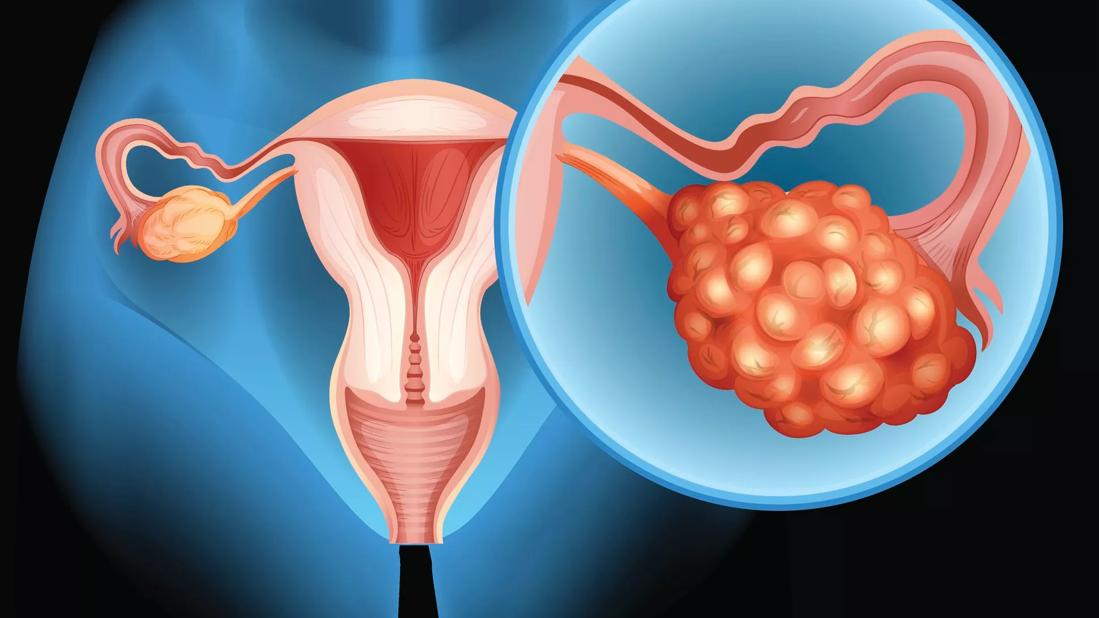
Previous research has demonstrated that antibiotic treatment drives up resistance to platinum chemotherapy and immunotherapy in patients with melanoma, lung cancer and renal cell carcinoma. Its effects on EOC had not been known until now, even though it is a particularly dangerous form of cancer. Ovarian cancer overall (90% of which are EOC) is the most deadly gynecological cancer in the U.S., in part because it is often found so late: four out of five women diagnosed with ovarian cancer are found to have advanced disease that has already spread into the abdomen, according to the American Cancer Society. The National Cancer Institute estimates that 21,750 will be diagnosed with ovarian cancer in 2020, and 13,940 will die of it this year, making up 2.3% of all cancer deaths in the U.S.
Advertisement
While Dr. Vargas believes that more prospective studies are needed, these findings suggest that that doctors should be judicious in their use of antibiotics in EOC patients undergoing platinum chemotherapy, making absolutely sure that the treatment is necessary and that antibiotics are de-escalated where appropriate. That includes acute-care scenarios such as emergency rooms, who will most likely see EOC patients and are faced with making the initial decision to start antibiotics.
These findings could also bring changes to standards in cancer care. For example, Dr. Vargas said that antibiotics are often prescribed for neutropenia, which is low white blood cell count and common with chemotherapy and radiation, to prevent infections. “There is no strong evidence that antibiotic therapy as prophylaxis helps patient, and now there is this strong association that antibiotics may impact overall cancer prognosis and survival for a wide range of patients receiving PC,” he says. “If there’s no data to support it, and it may hurt patients in the long run, then we should exercise caution until prospective studies are completed.”
While antibiotic use and platinum resistance might be linked, this concept is still considered a hypothesis. Dr. Chambers believes that it may be related to the effect of these medications on gut microbiome, which she is currently studying using animal models.
Chemotherapy resistance, specifically platinum resistance may be tied to dysbiosis, which is a microbial imbalance that many people have already experienced as gastrointestinal distress after taking an antibiotic. While annoying, it’s not often a deadly side effect in otherwise healthy adults, but could be driving this resistance to treatment.
Advertisement
“Over the last decade, there’s been this increasing focus on the gut microbiome as responsible for people’s overall health, including for diseases like cancer,” Dr. Chambers says. “We think that the bacteria may act as a mediator for certain types of cancer treatments, including immunotherapy.”
Advertisement
Advertisement

Multidisciplinary teams work together in in-situ scenarios

Uterine transposition cleared the field for radiation therapy

ACOG-informed guidance considers mothers and babies

Prolapse surgery need not automatically mean hysterectomy

Artesunate ointment shows promise as a non-surgical alternative

New guidelines update recommendations

Two blood tests improve risk in assessment after ovarian ultrasound

Recent research underscores association between BV and sexual activity