Are outpatient hernia repairs around the corner?

With hernia repair the most common general surgery performed in the U.S. today, technology that may reduce pain or convert an inpatient surgery to outpatient merits a close look. Toward this end, Ajita Prabhu, MD, a specialist in minimally invasive surgery, is studying Cleveland Clinic’s use of robots in intraperitoneal mesh placement (rIPOM) as an alternative to the laparoscopic procedure (LapIPOM) for a subset of hernia repair candidates.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Dr. Prabhu performs up to four robotic hernia repair procedures a week. She is also a pioneer in rIPOM research and was recently published in the Journal of the American College of Surgeons. Her retrospective study sought to delineate the variances in 30-day outcomes between patients undergoing LapIPOM and rIPOM surgeries for small to medium-sized incisional hernia repair.
To do this, she analyzed data from 454 LapIPOM and 177 rIPOM cases. Results showed a reduced LOS with rIPOM, from 1 to 0 days. rIPOM patients also had a lower rate of SSOs (5% vs. 14%) and lower rate of complications from all causes, (9% vs. 18%), though most of the complications were seromas that resolved without intervention. Postoperative 30-day outcomes were virtually the same. SSOPI rates were very low and similar between the two groups.
The rIPOM procedure was longer, with 47 percent of the surgeries exceeding two hours, vs. 31 percent in the LapIPOM group. Dr. Prabhu suspects that “since the robots have only been used routinely for hernia repair since 2011 or 2012, it is likely that most of the surgeons were all somewhere on the learning curve.” This likely impacted the length of the surgery, something Dr. Prabhu thinks will decline when more surgeons perform a higher volume of cases.
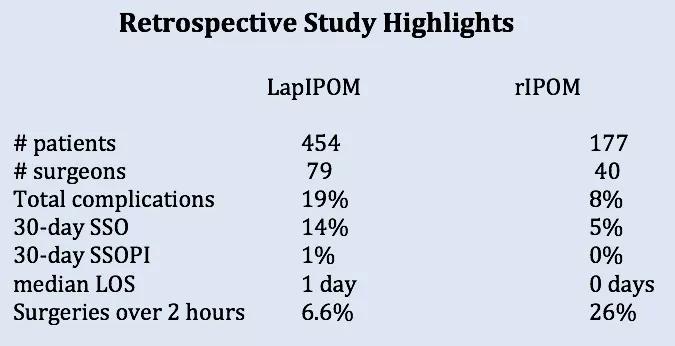
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/0a605aad-04d2-4a42-af97-198459bc22f6/17-DDI-3316-Prabhu-CQD-chart_jpg)
“I think there are some advantages to the technology. It allows us to do some things on a minimally invasive basis we couldn’t otherwise do, or would struggle to do.” Dr. Prabhu elaborates: “The robot has wristed instrumentation, allowing 360 degree motion, making it much easier to suture mesh in place without using mechanical fixation. Laparoscopy is a wonderful tool in the right hands, but it is difficult to get really good at the manipulations required for suturing mesh implants.”
Advertisement
Based on her patients’ feedback, Dr. Prabhu conjectures that the avoidance of mechanical fixation may explain the reduced pain patients perceive, enabling an earlier discharge. While research on rIPOM is scarce, another study comparing robotic with open retromuscular ventral hernia repair also found a shorter LOS and similar 30-day outcomes between the two groups. The authors suggested that the avoidance of mechanical fixation devices was a likely factor in lower LOS.
Dr. Prabhu elects rIPOM at every appropriate opportunity and has been steadily ramping up the volume over the year she has been with Cleveland Clinic. “I’m seeing patients go home sooner. This is a compelling reason to opt for rIPOM.”
Currently, every patient she operates on is being entered into the Americas Hernia Society Quality Collaborative database for follow-up. She explains, “There is so little research out there. We want to be the people to fill the knowledge gap.”
Dr. Prabhu is looking forward to studying this same application of rIPOM in a prospective manner to see if she can corroborate the findings from her retrospective study. “This study gives us the first early inkling that there is a benefit to rIPOM. I’m trying to evaluate this technology and see if it is relevant and has a space in our world. Time will tell, but this early data supports a call for continued research.”
Advertisement
Advertisement

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Potentially cost-effective addition to standard GERD management in post-transplant patients

Findings could help clinicians make more informed decisions about medication recommendations

Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care

Retrospective analysis looks at data from more than 5000 patients across 40 years

Surgical intervention linked to increased lifespan and reduced complications