Using novel robotic approaches for a difficult-to-access prostate
Excessive scar tissue in the abdomen has historically excluded patients from prostate surgery, owing to their higher risk of bowel injury. But urologists at Cleveland Clinic are using a surgical technique made possible with the single-port (SP) robotic system to circumvent this area and safely gain access to the prostate.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“The SP robot has low-profile instruments that allow us to go through narrow areas that otherwise are prohibitive with the multiport robot’s comparatively bulky instruments,” explains Jihad Kaouk, MD, Director of the Center of Advanced Robotic and Image-Guided Surgery at the Glickman Urological & Kidney Institute. The single-arm allows 360-degree multi-quadrant access. This design enables the robot to operate in a smaller anatomical space.
Applying this technique to patients with a hostile abdomen is the latest adaptation of the SP robot from Dr. Kaouk and team. Over the last several years, the robotic technology has made way for modified surgeries and new approaches that allow urologists to perform radical prostatectomy extraperitoneally (Figure 1), avoiding the sac that contains the bowel, and transvesically (Figure 2), surgical access to the prostate directly through the bladder.
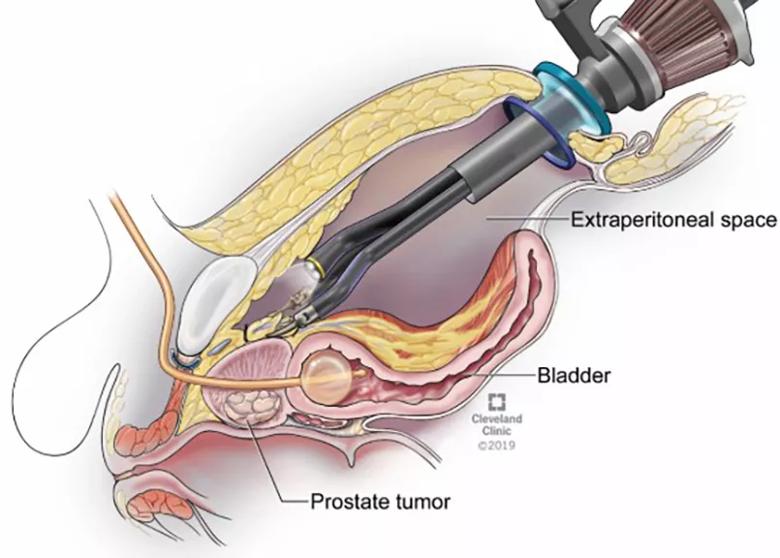
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/fa9c5237-c429-4c12-9abe-74ab18f48e25/23-URL-3796162-CQD-Inset2_jpg)
Figure 1. Extraperitoneal Single-Port Radical Prostatectomy. Note the surgical space above the bladder but outside the peritoneal sac.
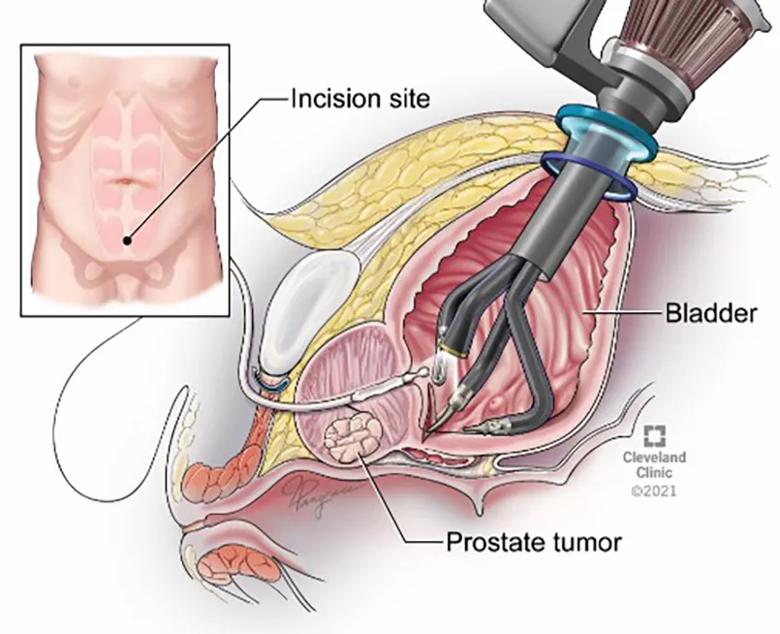
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/2fb73253-7582-4591-936d-e04fffde9251/23-URL-3796162-CQD-Inset1_jpg)
Figure 2. Transvesical Single-Port Radical Prostatectomy. Note the robot is introduced directly through the skin into the bladder.
These SP approaches have demonstrated improved recovery times, low complication rates and decreased operative pain, resulting in limited use of opioids for pain control. SP transvesical prostatectomy, typically indicated for patients with lower-risk prostate cancer and prostates less than 100 grams, has shown improved postoperative urine control. Both techniques were first described by Dr. Kaouk and team and were published in peer-reviewed journals.1-2
Advertisement
“In our latest series, we were able to avoid the entire amount of scar tissue by navigating around the abdomen. So, this approach allows us to reach the prostate to do an effective prostatectomy without the need for lysing of adhesions or increasing the risk of bowel injury,” explains Dr. Kaouk. He presented the team’s initial experience at the 2023 American Urological Association Annual Meeting in Chicago.
Dr. Kaouk explains: “During the transvesical approach, the bladder is entered through one incision and a gas bubble is created within the bladder. The surgeon introduces a camera and three other narrow-profile instruments through one cannula, where the gas bubble is limited, and the prostate surgery is done from within the bladder. To reestablish the urine path, the anastomosis is also done from within the bladder to the urethra.” He says patients have experienced very low morbidity from this procedure, resulting in the following:
Beyond patients who have surgery-prohibiting scar tissue—others have variation in their anatomy, such as a prominent pubic bone or wide dorsal vein complex. Others may have undergone attempted radical prostatectomy that was ultimately aborted by their physician for various complications.
Advertisement
The most significant subset of patients in the series has undergone J-pouch surgery, also known as ileal pouch-anal anastomosis, a procedure performed after a patient has had a proctocolectomy to create a pouch out of part of the small intestine.
“Because the prostate sits deep in the pelvis on top of the rectum, it’s extremely difficult to access due to adhesions, particularly in patients who have undergone J-pouch surgery, but this procedure makes it possible. So far, we’ve done nearly 50 patients with this type of clinical history,” notes Dr. Kaouk.
He says they’re serving a group of patients who have otherwise “run out of options.” The J-pouch surgery may relocate the bowel closer to the prostate, making radiation therapy a riskier proposition out of concern for inadvertently radiating the bowel during treatment. In the absence of surgery or radiation therapy, hormonal therapy is usually the only option for these patients, suboptimal for local cancer.
“We’ve continued to demonstrate the benefit of this new-generation robot with respect to regionalizing urologic surgeries. But, most of all, we are exceedingly pleased to improve access to treatment for patients who were previously not eligible for a radical prostatectomy because of a hostile surgical abdomen.”
References
Advertisement
Advertisement

Approach offers a ‘middle ground’ between radical prostatectomy and active surveillance

AI histologic classifier reliably predicts clinical risk in men post-prostatectomy

Historic collaboration connects two Cleveland Clinic locations, enables real-time sharing of metrics and surgical progress
Patient factors and cancer characteristics are key to deciding between focal therapies and whole gland treatment

Novel research to evaluate noninvasive treatments in ED and chronic pelvic pain
Correlation found between the biomarker HSD3B1 and resistance to combined hormone therapy and radiotherapy

FDA-approved therapy offers promise for patients with castrate-resistant prostate cancer

A newer modality for select patients has shown positive outcomes to date