Extent of baseline burden impacts progression-free and overall survival
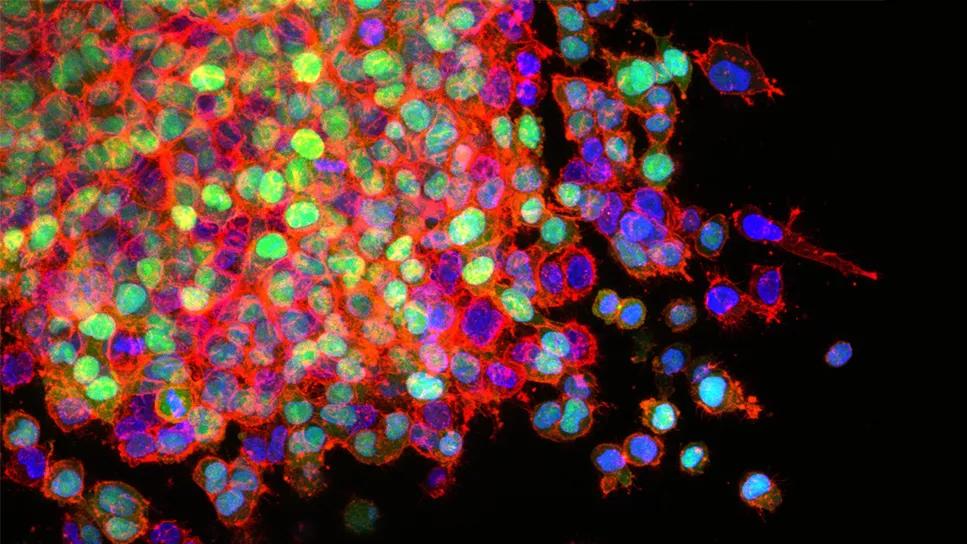
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/8d601c7f-bbf6-42c3-88eb-ea2ba49d1622/lung-cancer-cells-metastatis)
Lung cancer cells
The number of visceral tumors and metastatic disease sites impacts survival in patients with stage IV EGFR-mutant (EGFRm) non-small cell lung cancer (NSCLC) treated with osimertinib monotherapy, according to a Cleveland Clinic study recently presented at the American Society of Clinical Oncology 2024 annual meeting.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Traditionally, we’ve given osimertinib as monotherapy for these patients,” says Nathan Pennell, MD, PhD, co-director of the Cleveland Clinic Lung Cancer Program and Vice Chair of Clinical Research for Cleveland Clinic Cancer Center. “But recent trial data from FLAURA2 demonstrated a significant progression-free survival benefit to combination therapy with platinum-pemetrexed chemotherapy. Unfortunately, it also demonstrated a clear increase in adverse events, so it’s not a clear-cut decision. Our analysis offers an additional data point when considering this clinical decision.”
Acquired resistance to the tyrosine kinase inhibitor (TKI) osimertinib has remained a challenge for treating patients with EGFRm NSCLC. Some studies have indicated a potential association between tumor burden and the risk of developing resistant clones to TKI monotherapy, but none have explored an association with clinical outcomes.
The research team, including first author Lukas Delasos, DO, a fellow at Cleveland Clinic Cancer Center, reviewed the records of stage IV EGFRm NSCLC patients who received osimertinib between 2018 and 2023. Patients who discontinued use for reasons other than disease progression were excluded. The 325 patients had a median follow-up time of 22.7 months (0.6 – 85.6 months). Median progression-free survival (PFS) for the group was 16.3 months (95% CI; 13.7 – 18.9), and median overall survival (OS) was 31.1 months (95% CI; 27.4 – 39.3).
The team used the total number of visceral tumors (TTn, 1-4, 5-9, ≥10) and the total number of sites of metastatic disease (MDn, 1-2, 3-4, ≥5) to characterize tumor burden at baseline. Patients with 1-2 metastatic disease sites had better median PFS and OS compared with those with higher MDn of 3-4 and ≥5 (median PFS: 21.5 vs 11.4 vs 9.0 months, respectively [P < 0.0001]; median OS: 44.3 vs 20.8 vs 22.4, respectively [P < 0.0001]. A similar correlation was observed with the total number of visceral tumors; patients with 1-4 visceral tumors had significantly higher median PFS compared with patients with 5-9 and ≥10 visceral tumors (median PFS: 21.5 vs 16.3 vs 13.4 months, respectively P = 0.001). Patients with 10 or more visceral tumors had significantly worse median OS compared with those with 1-4 or 5-9 tumors (23.7 vs 35.1 vs 57.7 months, respectively; P < 0.0001). Location of metastases impacted survival as well, as patients with bone and liver metastases had worse median PFS and OS, and those with brain and lung metastases only had worse median OS.
Advertisement
In this cohort, the extent of a patient’s baseline tumor burden impacted both PFS and OS in patients with stage IV EGFRm NSCLC who have been treated with osimertinib monotherapy. Patients with lower tumor burden, as characterized by TTn and MDn, appear to fare better than those with intermediate or higher tumor burden, and the risk of adverse events may outweigh the benefits of combination therapy in this population.
“Ultimately, this topic needs further study, including prospective trials,” says Dr. Pennell, “but for a clinician deciding whether to treat with TKI or combination therapy, it may be a good idea to include tumor burden when weighing risks and benefits for these patients.”
Advertisement
Advertisement
Treatment assigned FDA review date in June 2025
Cleveland Clinic, the University of Minnesota and University of Cambridge receive $1M grant to develop point-of-care biosensor for early detection and treatment personalization
Hybrid treatment model helps improve cancer care access
Resection, radiotherapy or ablation?
Quantum computing being studied as a means to help improve predictive performance, accuracy
Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy
Targeting DNMT1 shows promise in chemotherapy- and immunotherapy-resistant SCLC
New review published in Cancers suggests a synergistic benefit