Patients who pass SEP-1 in hospital less often
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/51747ab2-ae55-4f72-afdf-73c04e6a713d/18-PUL-195-SCCM-Hero-Image-650x450pxl_jpg)
18-PUL-195-SCCM-Hero-Image-650x450pxl
By Anita Reddy, MD, and Seth Bauer, PharmD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The Severe Sepsis and Septic Shock Early Management Bundle (SEP-1) is one of several efforts from the U.S. Centers for Medicare and Medicaid Services to combat the prevalence and mortality of sepsis as well as mitigate the cost burden upon the healthcare system. Sepsis is the leading cause of hospital readmission, a major factor in patient mortality and healthcare cost. To date, we have no evidence-based methods of reducing readmissions after a sepsis episode.
Our study, presented at the Society of Critical Care Medicine (SCCM) Annual Congress in February 2018, sought to determine if SEP-1 bundle compliance is associated with hospital readmission. We evaluated for SEP-1 eligibility patients admitted to a health system from October 2015 – May 2017 with administrative coding for sepsis during index hospital admission. We then analyzed whether patients passed or failed SEP-1 and the individual bundle element that lead to failure. We also looked at 30-day readmission. Note: the numbers below reflect the data as presented at SCCM. Updated analysis is forthcoming.
Of 1729 patients identified in the SEP-1 measure population, 34.5 percent passed SEP-1, and 90.3 percent survived index hospitalization. Hospital survival was 94.8 percent in patients who passed SEP-1 compared with 87.9 percent for those who failed (P < 0.01). Of the surviving patients, whose who passed SEP-1 had fewer readmissions than those who failed SEP-1.
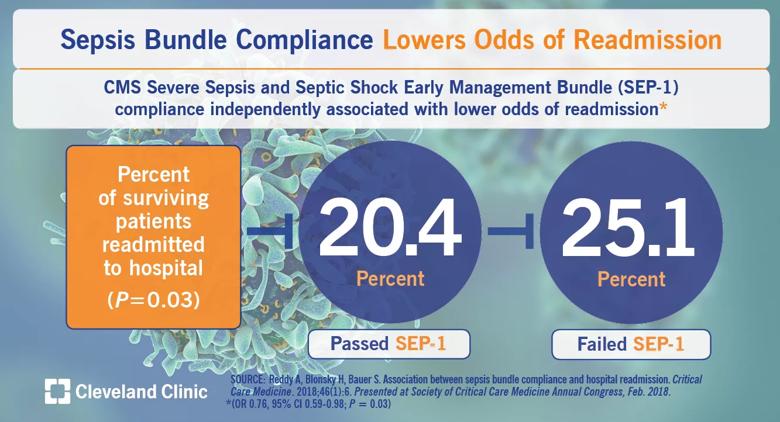
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5205c699-fa93-491e-8e00-980ec2096de1/18-PUL-234-SCCM-Visual-Abstract-1200x650pxl_02_jpg)
We analyzed individual elements of the SEP-1 bundle leading to failure, and none were associated with readmission. Using multivariate logistic regression, we found that SEP-1 compliance lowered odds of readmission (OR 0.76, 95% CI 0.59-0.98; P = 0.03).
Advertisement
As we search for interventions across the spectrum of sepsis prevention, treatment and mortality, compliance with the SEP-1 bundle may offer a targeted intervention that reduces admissions and decreases overall healthcare costs and sepsis disease burden beyond initial hospital admission.
Dr. Reddy is Quality Officer in the medical intensive care unit and Co-Chair of the Enterprise Sepsis Steering Committee at Cleveland Clinic. Dr. Bauer is a clinical pharmacist in the medical intensive care unit and a member of the Enterprise Sepsis Steering Committee at Cleveland Clinic.
Advertisement
Advertisement
Takeaways from the most recent annual meeting centered around clinical advances, AI integration and professional development
Recent breakthroughs have brought attention to a previously overlooked condition
A review of treatment options for patients who may not qualify for surgery
Looking at the real-world impact and the future pipeline of targeted therapies
The progressive training program aims to help clinicians improve patient care
New breakthroughs are shaping the future of COPD management and offering hope for challenging cases
Exploring the impact of chronic cough from daily life to innovative medical solutions
How Cleveland Clinic transformed a single ultrasound machine into a cutting-edge, hospital-wide POCUS program