A decade-old trial holds useful insights for current debates
To help make sense of recent studies of the management of stable coronary artery disease (CAD), cardiologists would do well to look to a major study from the recent past — the COURAGE trial, published in the New England Journal of Medicine in 2007. So argues Cleveland Clinic cardiologist Umesh Khot, MD, in a recent editorial in the Cleveland Clinic Journal of Medicine.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
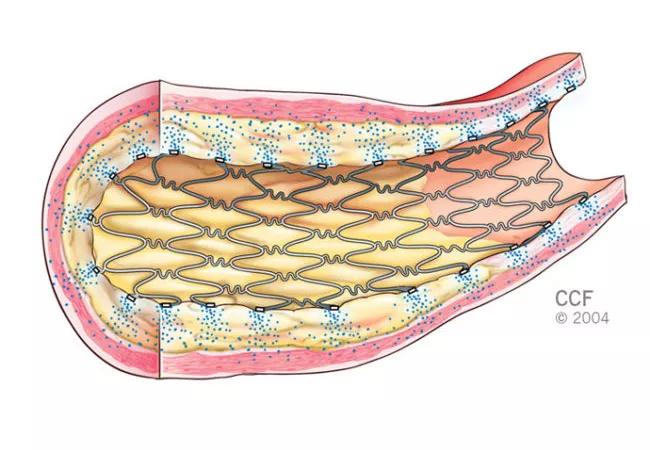
“A balanced approach to recommending PCI [percutaneous coronary intervention] first vs. optimal medical treatment first remains the best strategy” for patients with stable angina, writes Dr. Khot.
COURAGE was notable for showing that PCI did not reduce the risk of death or myocardial infarction (MI) in patients with stable CAD compared with a strategy of optimal medical therapy first. Its findings were heeded, Dr. Khot notes, as the rate of PCI use in this population plummeted in the wake of the trial, declining 60 percent from 2006 to 2011.
Yet Dr. Khot contends that claims that the COURAGE results were “negative” for PCI in stable CAD would be simplistic, in light of the following nuances:
Advertisement
For these reasons, Dr. Khot argues, “[i]t is more accurate to say that in selected patients with moderate symptoms of angina and without heart failure or left main artery disease, a PCI-first strategy has no advantage over an optimal medical treatment-first strategy for the risk of death and myocardial infarction but does lead to earlier angina relief and less long-term need for medication.” Additionally, he notes, an optimal medical treatment-first strategy fails and requires crossover to PCI in up to one-third of cases.
Three other observations are relevant to interpreting the COURAGE trial’s results, he points out:
Advertisement
All these observations led Dr. Khot to propose in his editorial a three-step approach to counseling patients with stable CAD on their treatment options:
He concludes that this type of “patient-centered approach to clinical decision-making mandates inclusion of PCI first as an option in the management of stable coronary artery disease.” For most patients with heart failure, class IV angina at rest or left main artery stenosis, he says, referral for revascularization will be indicated. For the remaining patients with confirmed CAD and moderate angina symptoms, decisions should be driven by coronary anatomy, symptom burden and patient desires.
Read the full editorial in Cleveland Clinic Journal of Medicine (2018;85:124-127).
Advertisement
Advertisement

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients

Multimodal evaluations reveal more anatomic details to inform treatment

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more