New tools to teach an old procedure
By Neal F. Chaisson, MD; Eduardo Mireles-Cabodevila, MD; Rendell Ashton, MD; Aanchal Kapoor, MD; Abhijit Duggal, MD; Anirban Bhattacharyya, MD; Siddharth Dugar, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In 2014, the Accreditation Council for Graduate Medical Education (ACGME) published recommendations for entrustable professional activities (EPAs), which are areas of procedural and cognitive proficiency expected of trainees who completed specialty or subspecialty training. For critical care and pulmonary/critical care trainees, the current EPAs include proficiency in placing and interpreting data from a pulmonary artery catheter (PAC).
Historically, PAC placement was a common procedure in intensive care units. A series of studies demonstrating that routine use of PACs do not improve clinical outcomes led to a significant decline in their use. Nonetheless, in select patients, such as those with pulmonary hypertension, use of a PAC to guide management is still recommended.
In a 2013 survey of pulmonary and critical care program directors, several concerns were raised with regard to the current state of training in PAC placement and use. Fifty-four percent of respondents estimated that current fellows perform less than 10 PACs during fellowship, and 57 percent suggested that PAC training was inadequate. Eighty-one percent of respondents agreed that proficiency in PAC data interpretation should be an ACGME requirement.
When we reviewed our program’s training methods for PAC placement and management in 2014, we realized we were no different. Teaching was sporadic and did not follow a well-formed curriculum. Experience with PAC use among fellows was low, and less than 40 percent of our fellows felt confident in using PACs.
Advertisement
To address this issue, we devised an educational curriculum to provide didactic and hands-on training in the proper use and interpretation of PACs, arterial catheters and echocardiograms for shock assessment.
Our curriculum included three components:
1. A series of online modules reviewing heart-lung physiology and hemodynamic waveform interpretation.
2. Four lectures on the physiology of shock.
3. A one-day simulation course to integrate principles learned in the modules and lectures with hands-on procedural training.
As part of the course, our team developed a right heart catheter insertion simulator from moldable plastic, a clear plastic bottle and Foley catheter tubing. Although the product was rudimentary, trainees felt it offered valuable instruction on how to correctly place a PAC.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/09379c98-9226-4994-9d03-905d5cbc564d/CQD_18-PUL-441_inset_1_850_jpg)

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5c4cb910-a6d1-4b49-a933-c4e2a6ee0e08/figure-1-2_png)
Initial models of the right ventricle were attached to a pulmonary circuit. Vessels within the pulmonary circuit were tapered to allow wedging of the PA catheter during insertion.
In subsequent years, we have made major improvements and now have two PAC task trainers. The first, which includes a 3D-printed model of the right atrium, ventricle and pulmonary arteries, represents a more sophisticated version of our first simulator and allows learners to visualize the concept of PAC insertion, flotation and wedging.
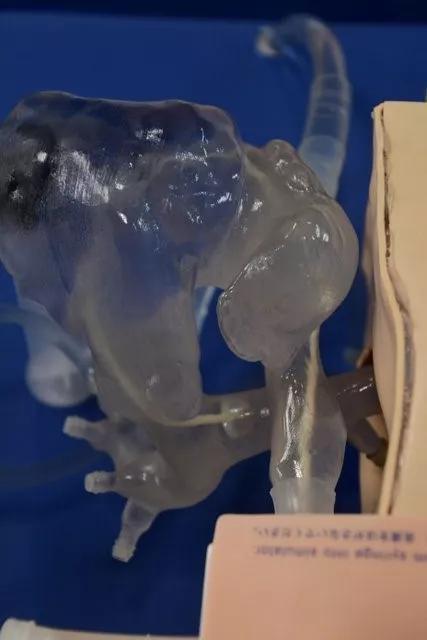
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e21275db-062c-444d-b6b5-1ed8161bedf0/inset-4_jpg)

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/ea6ad4d5-7deb-4c4c-929a-d0c7c9fc5b27/inset-3_jpg)
Learners insert a Swan-Ganz catheter through an introducer sheath in the neck of the simulator. The current right ventricle was developed using reconstructed CT scan images and a 3D printer.
Advertisement
The second, a PAC waveform simulator, helps learners review waveforms associated with PAC placement and visualize wedging technique and thermodilution cardiac output.
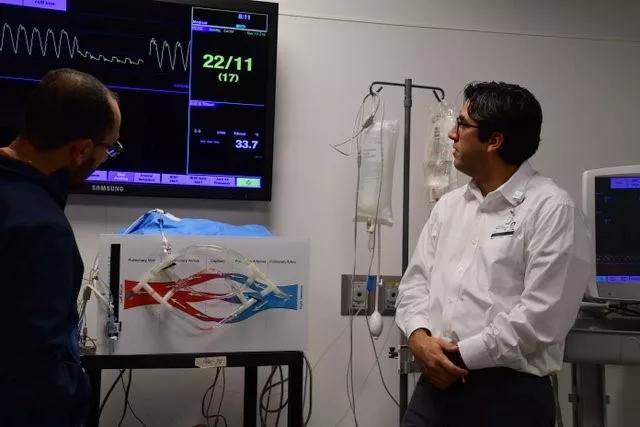
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/f00ee948-b12b-47fa-b3b0-4c96c6ed85d0/inset-5_jpg)
A second task trainer generates waveforms one would see as a PA catheter is inserted from the right atrium to the pulmonary arteries. This trainer allows learners to review waveforms associated with PAC placement, to visualize the effects of wedging and perform thermodilution cardiac output measurements.
As a result of these simulation improvements, 89 percent of our trainees now agree or strongly agree that they can safely insert a PAC and interpret data for assessment of shock. Eighty-two percent of fellows agree or strongly agree that they can safely troubleshoot a PAC without assistance.
Beyond the use of these simulators to train our fellows, we have had opportunities to utilize these tools in other educational settings. We added PAC simulation training to our medical student hemodynamics curriculum in 2018, and it was heralded as a best practice model in medical school education by the Dean’s Office. We have collaborated with industry to provide a workshop on hemodynamics for medical science liaisons and pharmaceutical representatives involved in the area of pulmonary hypertension. Feedback from these sessions has been uniformly positive, and these workshops are now a major educational component of our pulmonary hypertension program.
Although our PAC simulators have improved the educational experience well beyond our initial goals, the future holds additional opportunities. The next generation of PAC simulator — to be completed by late 2018 — will combine the two prior models and will allow learners to interpret both normal and abnormal PAC waveforms. It will also provide a simulation-based mechanism for ICU nurses to review proper PAC insertion, maintenance and data collection. Continued enhancements to the modules within our hemodynamics curriculum will be rolled out in 2019. We look forward to those opportunities as we work to further the education of those who serve, one of the founding tenets of Cleveland Clinic.
Advertisement
Dr. Chaisson directs the Critical Care fellowship program. Dr. Mireles-Cabodevila is Director of the main campus Medical Intensive Care Unit. Dr. Ashton is Education Officer for the Respiratory Institute. Dr. Kapoor directs the Medical Intensive Liver Unit. Dr. Bhattacharyya was associate staff in the Department of Critical Care Medicine. Dr. Duggal isstaff in the departments of Pulmonary Medicine and Critical Care Medicine. Dr. Dugar is associate staff in the Department of Critical Care Medicine.
Advertisement
Advertisement
Takeaways from the most recent annual meeting centered around clinical advances, AI integration and professional development
Recent breakthroughs have brought attention to a previously overlooked condition
A review of treatment options for patients who may not qualify for surgery
Looking at the real-world impact and the future pipeline of targeted therapies
The progressive training program aims to help clinicians improve patient care
New breakthroughs are shaping the future of COPD management and offering hope for challenging cases
Exploring the impact of chronic cough from daily life to innovative medical solutions
How Cleveland Clinic transformed a single ultrasound machine into a cutting-edge, hospital-wide POCUS program