Revolutionizing pediatric urology with a new, less invasive approach

A 17-year-old male presented to the emergency department with right flank pain and nausea. He was referred to the Division of Pediatric Urology at Cleveland Clinic for evaluation of hydronephrosis, a condition characterized by a dilated kidney.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Jessica Hannick, MD, a pediatric urologist at Cleveland Clinic, notes that the patient’s symptoms were consistent with ureteropelvic junction (UPJ) obstruction. However, the clinical picture was complicated by a previous CT scan that lacked contrast, obscuring critical anatomical details.
Most cases of UPJ obstruction stem from congenital abnormalities, affecting approximately 1 in 500 live births. In older children and adolescents, however, this condition may arise from external factors such as compression by accessory blood vessels. Untreated obstruction can lead to significant kidney damage.
To clarify the diagnosis and assess kidney function, Dr. Hannick ordered a renal scan with furosemide. The diuretic-induced diuresis exacerbated the patient's pain, reinforcing the suspicion of UPJ obstruction. Subsequent evaluations revealed a “creatinine bump,” indicative of decreased kidney function, further supporting the diagnosis.
For symptomatic older patients, pyeloplasty is the standard intervention to remove the blockage. While many urologists typically utilize open or robotic-assisted multiport laparoscopic techniques, Dr. Hannick and her colleague John (Jack) Weaver, MD, identified this patient as an ideal candidate for another groundbreaking surgical option: single-port (SP) pyeloplasty.
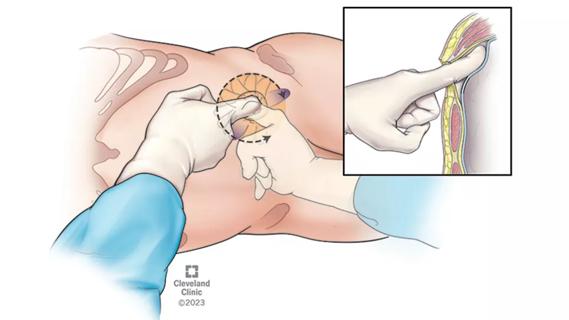
At Cleveland Clinic, Jihad Kaouk, MD, a leader in robotic urologic surgery and Director of the Center for Robotic and Image-Guided Surgery, recently pioneered a retroperitoneal low anterior access (LAA) technique, which enhances the advantages of the SP robotic approach in urologic surgeries, including pyeloplasty, partial nephrectomy and ureteral reimplantation.
Advertisement
This innovative SP robotic approach allows the surgical team to localize the procedure while avoiding the intraperitoneal space, a significant advancement over traditional multiport techniques that require multiple incisions in the abdominal cavity. Instead, the SP approach results in a single, small 3 cm incision.
Dr. Weaver highlights the importance of this innovation, noting, “It’s a game changer in terms of cosmesis and recovery. Since we’re not operating in the peritoneal space, there’s no risk of bowel herniation through the incision, which enhances patient safety.”
Utilizing the LAA technique further minimizes the invasiveness of the procedure by avoiding abdominal muscle dissection, resulting in reduced postoperative pain and quicker recovery times. Dr. Kaouk and his colleagues have documented successful outcomes using this method, including a non-narcotic pain management pathway and a same-day discharge protocol.
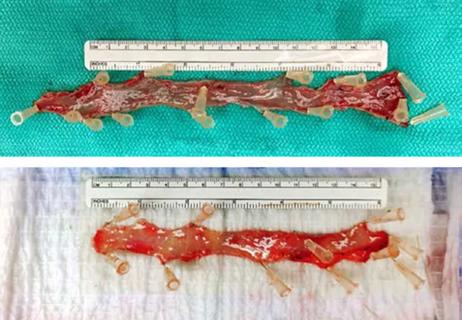
The surgery successfully addressed the patient’s ureteral obstruction. He was discharged home the same evening, equipped with a ureteral stent and without any additional drains.
During a follow-up appointment six weeks later, Dr. Hannick removed the stent. Three months post-surgery, an ultrasound confirmed the success of the repair, and the patient reported no further pain or nausea. Dr. Hannick plans to monitor his recovery for one year before transitioning him to an adult urologist.
“The incision looks remarkable; it’s virtually undetectable,” Dr. Hannick notes. “He is now 18, living the life of a typical teenager, and, most importantly, he is pain-free.”
Advertisement
Although this patient’s anatomy resembled that of a young adult, the pediatric urology team is determined to expand robotic surgical options for younger patients. While technical challenges remain due to smaller anatomical structures, the team is committed to refining and innovating robotic urologic surgeries for the pediatric population. To date, approximately 20 pediatric patients have successfully undergone SP urologic surgeries at the center, primarily for pyeloplasty and nephrectomy.
Dr. Weaver states, “Focusing on innovations, our mission is to adapt and replicate the successful techniques used in adult populations for our pediatric patients, ultimately enhancing outcomes and quality of care.”
Advertisement
Advertisement
The low anterior access approach using the single-port robot is gaining attention within the field

Retrospective study shows SGLT-2 inhibitors may lead to worse urologic outcomes

What it could mean for the future of ambulatory monitoring for bladder conditions
Study highlights benefits of nephrologist-led urine sediment analysis

Study reinforces the benefits of using cystatin C
Cleveland Clinic surgeons describe a new technique for harvesting a rectal mucosa graft

New study sheds light on national trends in urology residency, former CCLCM alum comments