35-year-old presents with suspected iris melanoma

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/f0a1a56b-2524-4d12-8595-aa2d75a3be11/EYE-2440858_10-07-21_009_RN-jpg)
Arun Singh, MD
A 35-year-old presented at Cole Eye Institute with a lesion in the left iris. He had been seen annually by an outside optometrist for seven years. The lesion had not been noted previously.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The patient did not have any visual symptoms, and his visual acuity was 20/20 in both eyes.
The elevated pigmented lesion in the iris was associated with nodularity along the pupillary margin between the 10- and 11-o’clock position. There were no feeder vessels or neovascularization of the iris on exam.
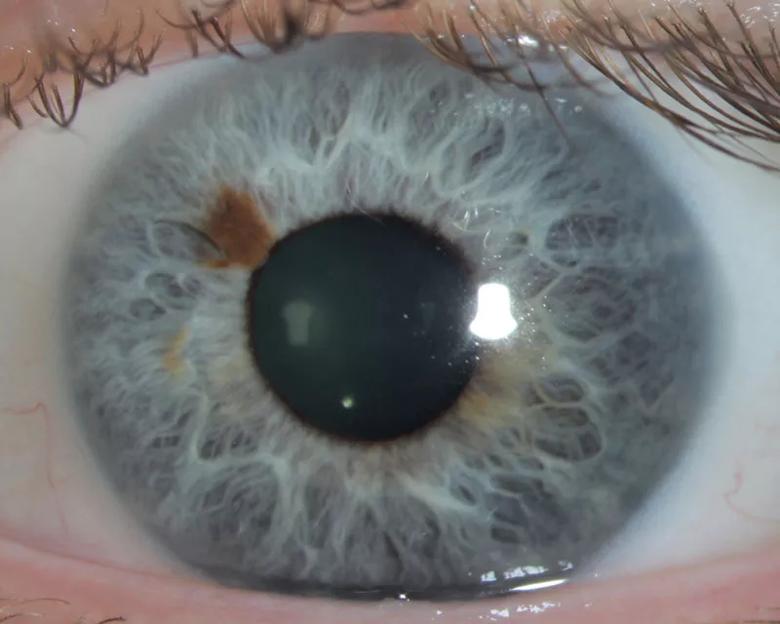
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/92af494b-e507-4093-9821-4e739a7bbb8d/20-EYE-1989584-CQD-Case-study-melanoma-Iris-Inset-1_jpg)
Anterior segment OCT showed multinodular iris thickening.
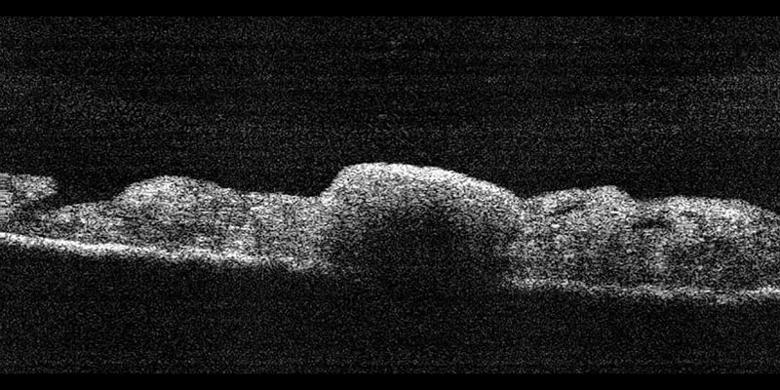
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/0bc97c82-347b-4b79-b7a2-a16f51cc8d3a/20-EYE-1989584-CQD-Case-study-melanoma-Iris-Inset-2_jpg)
Although the lesion was small and appeared like a nevus, melanoma was suspected due to recent onset.
“Freckles and nevi of the iris are very common,” says Arun D. Singh, MD, Director of Ophthalmic Oncology at Cole Eye Institute. “All spots aren’t malignant, but there are some clues that can indicate which spots likely are.”
According to Dr. Singh, iris lesions suspicious for melanoma are those that:
Following discussion of treatment options, the patient agreed to undergo excisional biopsy of the lesion with pupilloplasty using a small-incision approach.
Conventionally, iris resection for a suspected malignancy has involved a large incision in the cornea and sclera and the removal of 25% or more of the iris. This sector iridectomy has been associated with increased risk of wound-related complications, tumor seeding and recurrence, and photophobia due to iris defect.
Almost 15 years ago, Dr. Singh developed a new technique: small-incision guarded hydroaspiration (SINGH procedure). Instead of one large incision, there are multiple small incisions. After excising the tumor, plastic tubing containing a sodium hyaluronate solution is inserted into the anterior chamber. Using a syringe, the excised lesion is pulled into the tube, where it is isolated and removed safely as the tube is withdrawn from the anterior chamber. This prevents the tumor from being pulled across the wound, possibly shedding cells and seeding the edges of the wound.
Advertisement
The next step, pupilloplasty, restores the iris to a near-normal shape with a suturing slip-knot technique since the iris does not have capacity to heal. This restoration of the iris not only repairs the cosmetic defect but helps prevent photophobia.
“Healing was much slower — six weeks or longer — with conventional techniques using the larger incision,” says Dr. Singh. “Distortion of the cornea was a problem too. If you’d make a 6 mm wound in the cornea, it would be irregular when it healed. Multiple smaller incisions allow faster healing. Patients typically have normal vision within a week or so.”
In this case, as clinically suspected, histopathology confirmed iris melanoma. All surgical margins were negative.
One day later, the patient’s vision was 20/30 with minimal postoperative inflammation.
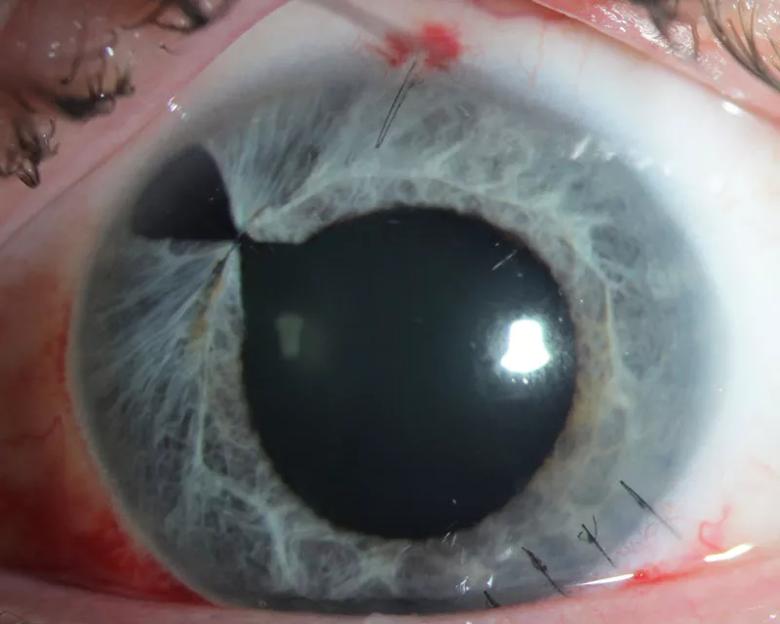
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/9b0f20df-0673-4f8f-afa8-123e98c4dfa7/20-EYE-1989584-CQD-Case-study-melanoma-Iris-Inset-3_jpg)
Four weeks following surgery, the patient’s vision was normal (20/20) without change in corneal astigmatism. The pupil size was equal between the two eyes in ambient light.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/4d8402da-5f51-4882-b0ae-21634d238725/20-EYE-1989584-CQD-Case-study-melanoma-Iris-Inset-4_jpg)
Now three years since surgery, the patient remains recurrence-free.
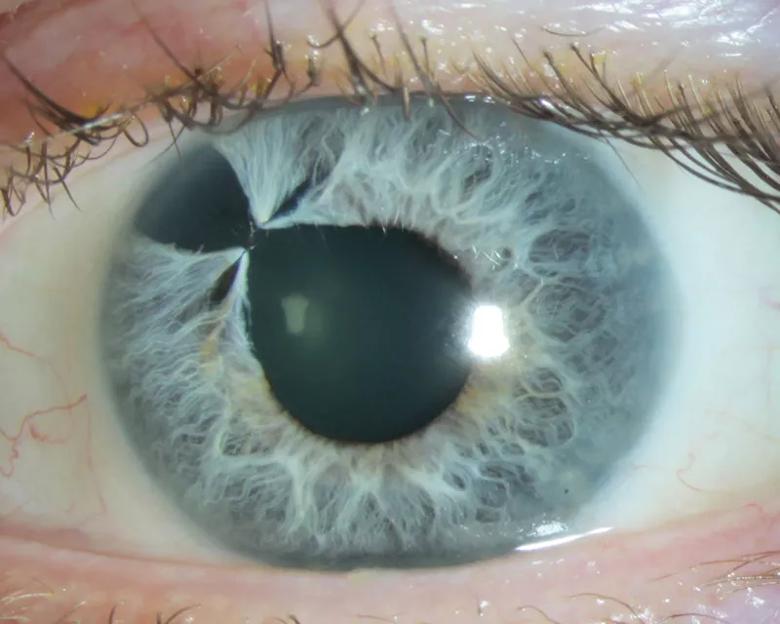
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/71d42421-8540-4052-b44a-4a7d9ffbcfca/20-EYE-1989584-CQD-Case-study-melanoma-Iris-Inset-5_jpg)
Melanoma of the uvea is rare, occurring in just six per 1 million people. Approximately 10% of uveal melanoma occurs in the iris — extremely rare.
Two decades ago, the only option for removing uveal melanoma was an iridectomy with a large corneoscleral incision, requiring six weeks or more of healing and slow visual recovery. New techniques and better instrumentation now provide another option, with a better risk-benefit ratio, says Dr. Singh.
“Today, if I see a lesion growing, I recommend we remove it because I know we can do so safely with minimally invasive techniques,” he says. “In the past, we would just watch the lesion and hope to avoid a big surgery.”
Advertisement
Even small lesions can be suspicious for melanoma, which can be removed easily with low risk to the patient, he concludes.
Advertisement
Advertisement
Goal-of-care discussions drive earlier hospice access
Clinical trials and de-escalation strategies
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting