The American Urological Association (AUA) is set to issue new guidelines in 2023 that could impact the use of transrectal biopsy (TR-Bx) for prostate cancer diagnosis, a technique that has fallen out of favor in Europe where transperineal biopsy (TP-Bx) is now the standard of care.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Board-certified urologist Alberto Pieretti, MD, with Cleveland Clinic Weston Hospital, hopes the AUA will follow the course of the European Association of Urologists (EAU), which issued a position paper in January 2021 making TP-Bx the preferred method in Europe.
“Transperineal biopsy should be the standard of care in the United States,” says Dr. Pieretti, who is fellowship-trained in urologic oncology and almost exclusively uses this approach in his practice. “It is associated with less complications and provides the same, if not more, benefit in diagnosing prostate cancer.”
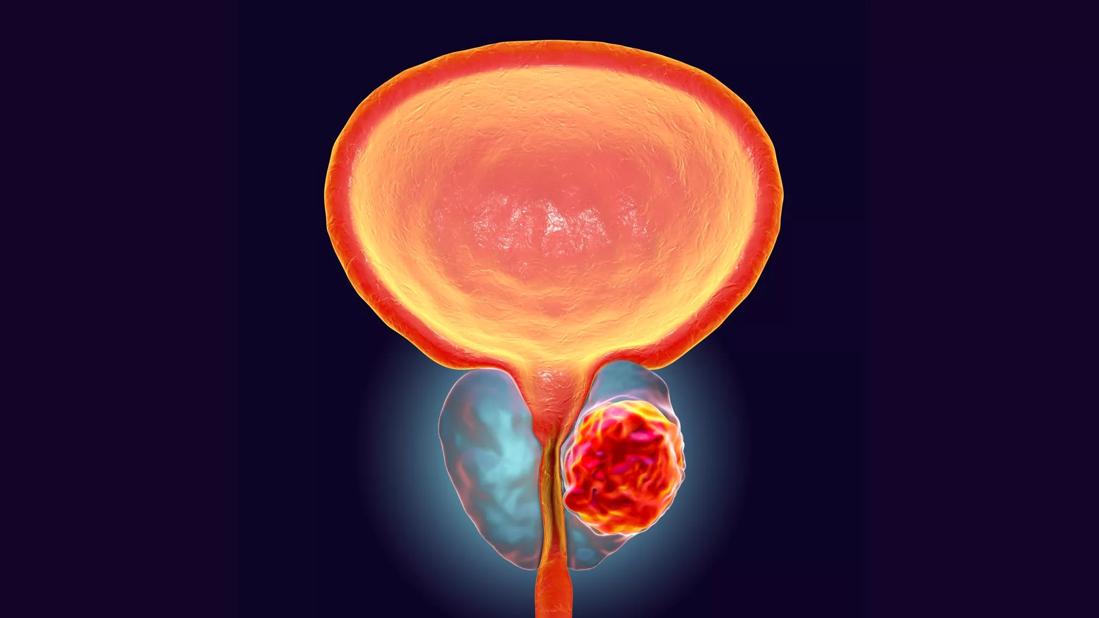
Approximately one million prostate biopsies are performed in the United States each year, and the vast majority are in-office procedures using a transrectal ultrasound (TRUS) approach. This method accesses the prostate through the rectal wall, which can push bacteria-ridden fecal matter into the sterile prostate gland and urinary tract, resulting in a greater risk of infection and sepsis.
“Even with antimicrobial prophylaxis, the post-transrectal biopsy infection rate is as high as 7%,” says Dr. Pieretti. “And an estimated 1 to 3% of transrectal biopsy cases lead to sepsis, which can result in severe complications and death.”
He notes the EUA policy shift addressed this safety issue and the growing concern of antibiotic-resistant organisms. “Studies have shown a link between the disturbing rise in sepsis rates in recent years and the increase in fluoroquinolone resistance,” adds Dr. Pieretti.
An increasing number of urologists are now performing transperineal biopsies, either in clinic with local anesthesia or the OR with sedation. The transperineal approach involves the insertion of the biopsy needle through the perineal skin and pelvic floor and into the prostate rather than the rectal wall. This decreases the chances of developing an infection and for rectal bleeding.
Advertisement
Multiple studies have demonstrated TP-Bx has a lower risk for post-biopsy infection, including one recently published in AUA News. It compared a number of biopsy techniques and found a significantly lower infection rate associated with transperineal MRI-ultrasound fusion guided prostate biopsy (1.3%) than with TRUS prostate biopsy (4%).
“My approach is to get a multiparametric MRI scan before the biopsy and then do transperineal fusion biopsies as a standard to minimize the risk of infections,” says Dr. Pieretti. He performs several a week at both Weston Hospital and Cleveland Clinic Florida Coral Springs and has a 0% post-biopsy infection rate.
Dr. Pieretti points to another advantage of transperineal biopsies — the ability to find more cancer. Studies of TP-Bx have found higher detection rates for prostate cancer compared to TR-Bx, particularly for anterior zone tumors. “The anterior aspects of the prostate and the apex are difficult to sample with a transrectal approach,” he observes.
This is demonstrated in an international, multicenter retrospective cohort study published last month in the Journal of Urology. It comprised 5,241 patients who underwent MRI-guided prostate biopsy across 10 tertiary referral centers between December 2014 and November 2020.
Results show transperineal MRI-targeted prostate biopsy improves detection of clinically significant prostate cancer over transrectal MRI-targeted prostate biopsy, especially in the apex, transition/central zone and anterior zones.
Advertisement
“This study found a 15% improvement in identifying clinically significant prostate cancer using the transperineal approach, which is a tremendous benefit for patients,” says Dr. Pieretti. “More than ever, patients should know their options.”
Small studies and anecdotal polling also demonstrate a patient preference for the transperineal approach when given the choice. A study in the May 2022 issue of Journal of Urology surveyed 49 patients who had undergone both types of biopsies and found 61% would prefer a TP-Bx if they required a repeat biopsy while 32.7% would choose TR-Bx.
Similarly, an informal poll at an AnCan event earlier this year found that 48% of respondents would choose the transperineal approach for their next biopsy and only 22% would opt for a transrectal approach. The remaining 30% had no preference or were unsure.
“Transperineal biopsy conveys too many important patient benefits to ignore,” says Dr. Pieretti. “I hope the new AUA guideline will reflect this mounting evidence and more urologists will embrace the technique. It’s what our patients deserve.”
Advertisement
Advertisement

Nonthermal technique reduces bleeding and perforation risk

Standardizing a minimally invasive approach for Barrett’s Esophagus and Esophageal Cancer

PSMA-targeted therapy for metastatic prostate cancer now offered at Cleveland Clinic Weston Hospital

Nationally recognized urologic oncologist offers vision for growth, innovation, and excellence

Noninvasive modality gains ground in United States for patients with early-to-moderate disease

Cleveland Clinic Weston Hospital’s collaborative model elevates care for complex lung diseases

Interventional pulmonologists at Cleveland Clinic Indian River Hospital use robotic technology to reach small peripheral lung nodules

Trained in the use of multiple focal therapies for prostate cancer, Dr. Jamil Syed recommends HIFU for certain patients with intermediate-risk prostate cancer, especially individuals with small, well-defined tumors localized to the lateral and posterior regions of the gland.