A growing number of patients are undergoing holmium laser enucleation of the prostate (HoLEP) for benign prostatic hyperplasia (BPH). The incisionless procedure has been historically underutilized despite offering several advantages over transurethral resection of the prostate (TURP), the most common surgery for enlarged prostates, and simple prostatectomy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Board-certified urologists Fernando Cabrera, MD, with Cleveland Clinic Weston Hospital, and Jamil Syed, MD, with Cleveland Clinic Indian River Hospital, are among a small number of urologists in Florida offering HoLEP for the surgical management of BPH.
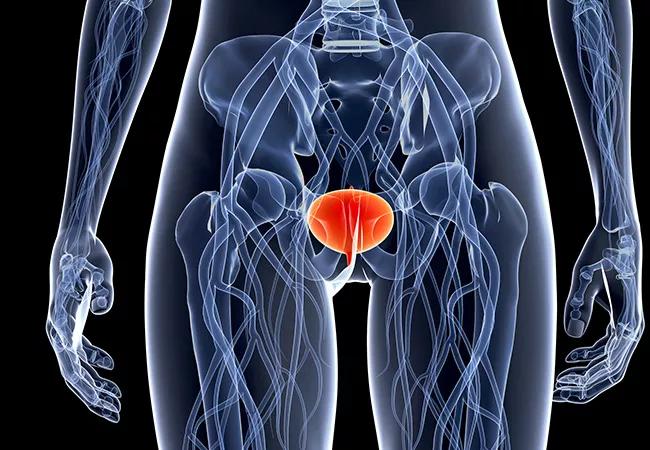
HoLEP is a minimally invasive procedure that uses a holmium laser to enucleate the prostate tissue, peeling it away from the surgical capsule. The hyperplastic tissue is pushed into the bladder and morcellated, where it can then be evacuated through the urethra.
Current American Urological Association (AUA) guidelines recommend HoLEP as a prostate size-independent treatment option for the surgical management of lower urinary tract symptoms (LUTS) associated with BPH.
“HoLEP is a versatile endoscopic procedure that I can use to treat most cases of BPH regardless of size, though it’s an especially good option for men with larger prostates,” says Dr. Cabrera.
HoLEP was first developed in the 1990s but was not widely adopted in the United States. More recently, technology advancements — including newer pulse modulated holmium lasers and a safer, more efficient morcellator — have renewed interest in the procedure.
“The newer generation of technology has decreased the operating time and improved hemostasis so that the majority of my patients go home the same day of their surgery and do not require a catheter,” reports Dr. Cabrera. He’s performed more than 300 cases since 2021, and now performs 7 to 10 cases a week.
In addition to being a safe, durable treatment option with a lower chance of retreatment, Dr. Cabrera points to the lower risk of injury and complications with HoLEP when compared to TURP and PVP and the reduced cost associated with the procedure. Research also has shown it to be more cost-effective than simple prostatectomy in cases of large or very large prostates.
Advertisement
“It’s a one-and-done procedure with a faster recovery and fewer complications,” adds Dr. Cabrera.
According to a retrospective cohort analysis published this year in the Journal of Endourology, adoption of HoLEP is on the rise in the U.S., increasing from 4.8% in 2015 to 7.6% in 2020. Using American College of Surgeons National Surgical Quality Improvement Program data from 2011 to 2020, the researchers also noted, compared to other BPH treatments, HoLEP cases had significantly lower complication rates, including urinary tract infections, blood transfusions, 30-day readmission, and reoperation.
Another study published in 2023 looked at data from the Nationwide Ambulatory Surgery Sample to evaluate BPH surgery uptake trends. The researchers found HoLEP accounted for 8.3% of all ambulatory BPH surgeries in 2019 up from 4.7% in 2016, surpassing photoselective vaporization of the prostate (PVP) as the second most common surgery behind TURP.
“While the number of HoLEP cases are still relatively small to date, I think more patients will start asking for this option over other surgical approaches especially as more urologists undergo training,” says Dr. Cabrera.
HoLEP is a specialized procedure that requires intensive training, but few urologists and institutions in the United States currently teach and perform it. According to a survey conducted by researchers with the Glickman Urological and Kidney Institute at Cleveland Clinic, only 12% (6/49) of U.S. endourology fellowships included HoLEP in their training as of 2019.
Advertisement
“This procedure has a steep learning curve and requires an investment in technology, which has hindered its adoption,” notes Dr. Cabrera. “But we’re starting to see more fellowships offering the training required and more opportunities for urologists to learn HoLEP.”
He is confident HoLEP will continue to gain favor among urologists and patients, especially as some are already calling for the surgical treatment to become the new gold standard.
Advertisement
Advertisement

Nonthermal technique reduces bleeding and perforation risk

Standardizing a minimally invasive approach for Barrett’s Esophagus and Esophageal Cancer

PSMA-targeted therapy for metastatic prostate cancer now offered at Cleveland Clinic Weston Hospital

Nationally recognized urologic oncologist offers vision for growth, innovation, and excellence

Noninvasive modality gains ground in United States for patients with early-to-moderate disease

Cleveland Clinic Weston Hospital’s collaborative model elevates care for complex lung diseases

Interventional pulmonologists at Cleveland Clinic Indian River Hospital use robotic technology to reach small peripheral lung nodules

Trained in the use of multiple focal therapies for prostate cancer, Dr. Jamil Syed recommends HIFU for certain patients with intermediate-risk prostate cancer, especially individuals with small, well-defined tumors localized to the lateral and posterior regions of the gland.