Study underscores the magnitude of stroke in pediatric ECMO patients

By Chidiebere Ezetendu, MD; Orkun Baloglu, MD; Hasan F. Othman, Vanishree Nandakumar, Samir Latifi, MD; and Hany Aly, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Pediatric extracorporeal membrane oxygenation (ECMO) has come a long way since its first use in an infant with persistent pulmonary hypertension in 1975.1 As of 2017, over 38,000 neonates have been supported with ECMO for cardio-respiratory and resuscitative causes.2 Despite the advances in critical care, the use of ECMO continues to save many high-risk patients. One of the most serious complications encountered in patients during ECMO support is cerebrovascular accidents, or stroke. The investigators at Cleveland Clinic Children’s utilized the largest publicly available inpatient database, the National Inpatient Sample (NIS), to study the prevalence of stroke in pediatric ECMO patients.
Stroke is known to cause cognitive deficits, long lasting seizure disorder, and, when occurring early in life, developmental delay may take place.3 There are two types of stroke that can occur during ECMO: hemorrhagic stroke and ischemic stroke. Hemorrhagic stroke is mainly attributed to the use of systemic anticoagulation during ECMO and the exposure of blood to the extracorporeal circuit, which can initiate a coagulation cascade.4 Ischemic stroke is related to the compromised perfusion of the brain in these patients who are practically in shock. These two types are not mutually exclusive as some patients may have both types of stroke. This study assessed the prevalence, mortality and comorbidities associated with stroke in pediatric ECMO patients.
A total of 114,477,997 records were reviewed. Overall, 28,695 (0.025%) pediatric ECMO patients were identified, of which 2,982 (10.4%) had a stroke and were further classified as hemorrhagic (N = 1,464, 49%), ischemic (N = 1,280, 43%) or combined (N = 238, 8%). There were no significant ethnic or gender differences in the frequency of stroke in the study population.
Advertisement
The overall prevalence of stroke was 10.4%, with more prevalence in patients older than one year of age (15.4%) as compared to only 8.6% in patients < 1 year of age. Stroke was most prevalent in patients with congenital heart diseases; this was encountered in more than half of stroke patients (58%) in the sample. Other underlying morbidities in ECMO patients who developed stroke included hypertension, dysrhythmias, sepsis, and shock.
Pediatric patients with stroke supported with ECMO had higher mortality compared to patients without stroke (46.6% vs. 40.8%, odds ratio (OR) = 1.27, 95% confidence interval (CI): 1.18–1.37, P < 0.001) and longer median hospital length of stay (LOS) (33 vs. 27 days; P < 0.001) and higher costs of hospitalization ($692,475 vs. $465,513, P < 0.001). Among the subgroups, though hemorrhagic stroke was associated with highest mortality (53.8%), the longest hospital stay and highest costs were seen in the group with combined stroke (60 days and $879,816).
Trend analyses using Cochran-Armitage trend test indicated that ECMO use has significantly increased over the study years (2000-2017), and the mortality has significantly decreased. Nonetheless, the diagnosis of stroke in pediatric ECMO patients has significantly increased from 3.2% to 13.7% (Figure 1). The apparent increase in stroke diagnosis could probably be attributed to increased survival of ECMO patients with potentially longer ECMO duration or it may be a reflection of increased detection of stroke with improved bedside imaging. The apparent increase in stroke may also be related to the willingness to place more complex patients on ECMO and enhanced reporting of complications related to ECMO.
Advertisement
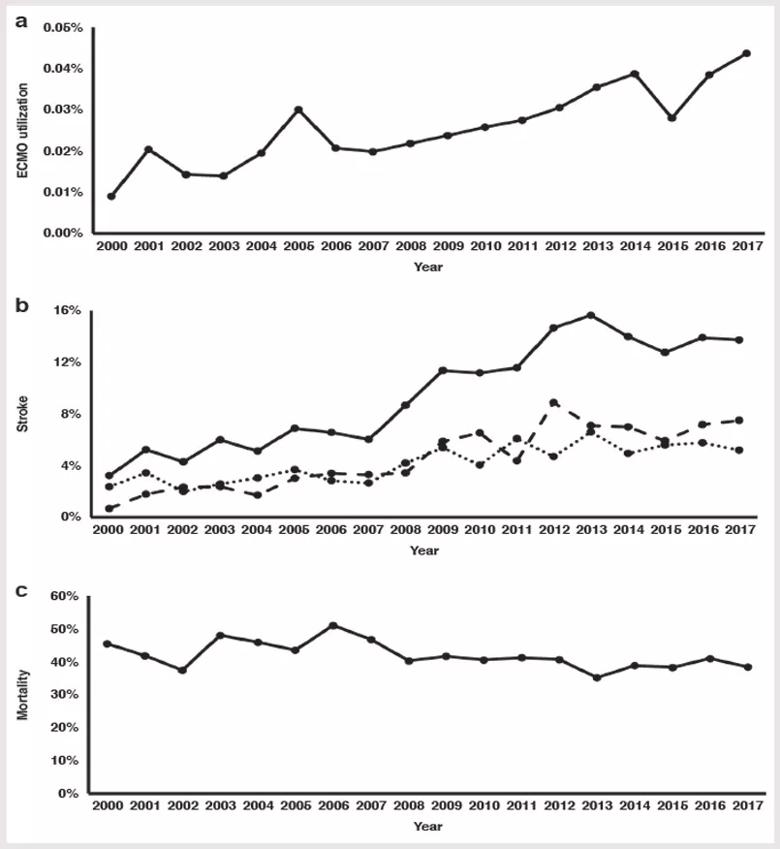
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/f2ff1cf6-4d85-4f8f-8fa0-c2d4ea0b51c2/22-CHP-3328148-Pediatric-Perspectives-DrAly-Stroke-in-ECHMO-inset_jpg)
Figure 1. Trends for pediatric ECMO utilization, survival and diagnosis of stroke during the study period. Panel a demonstrates ECMO utilization during the study period (2000–2017). Panel b represents stroke diagnosis for pediatric ECMO patients (solid line), including hemorrhagic stroke (dashed line) and ischemic stroke (dotted line). Panel c represents mortality trends during the study period. There were significant trends for increased ECMO utilization (P < 0.001), increased diagnosis of overall stroke and its two subtypes in pediatric ECMO patients (P < 0.001), and decreased ECMO mortality (P < 0.001). Reprinted with permission from the American Academy of Pediatrics. Figure appears originally in Ezetendu C, Baloglu O, Othman HF, Nandakumar V, Latifi S, Aly H. Stroke in pediatric ECMO patients: analysis of the National Inpatient Sample (NIS) database. Pediatr Res. 2022 Sep;92(3):754-761.
This study underscores the magnitude of stroke in pediatric ECMO patients, associated comorbidities and trends of ECMO use over the years. Further research is needed to actively mitigate modifiable risk factors of stroke and to enhance prevention and treatment of stroke in patients supported with ECMO.
About the authors: Dr. Ezetendu is staff in Cleveland Clinic Children’s Department of Pediatric Critical Care Medicine; Dr. Baloglu is Associate Staff; Dr. Latifi is Department Chair of Pediatric Critical Care; and Dr. Aly is Department Chair of Neonatology. Dr. Nandakumar is a scientific medical writer, and Dr. Othman was a former research fellow.
Advertisement
References
Advertisement
Advertisement

The progressive training program aims to help clinicians improve patient care

ECMO specialists partner with ethicists to guide fellow caregivers in critical decision-making

Aim is for use with clinician oversight to make screening safer and more efficient

Medical and surgical perspectives on current and emerging uses of ECMO and Impella

Quality improvement project addresses unplanned extubation

Tasked-based therapy improves social connection and quality of life

LAA closure may be compelling option in atrial fibrillation ablation patients at high risk of both stroke and bleeding

Case illustrates essentials of the low-risk, high-potential procedure when paired with rehab