Findings from a clinical trial and secondary analysis demonstrate clinical utility, safety
Findings from a phase IIa global trial found rituximab (RTX) to be generally safe, well-tolerated and effective in the treatment of granulomatosis with polyangiitis (GPA) or microscopic polyangiitis (MPA) in pediatric patients. The investigators reported their findings in Arthritis Rheumatology.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
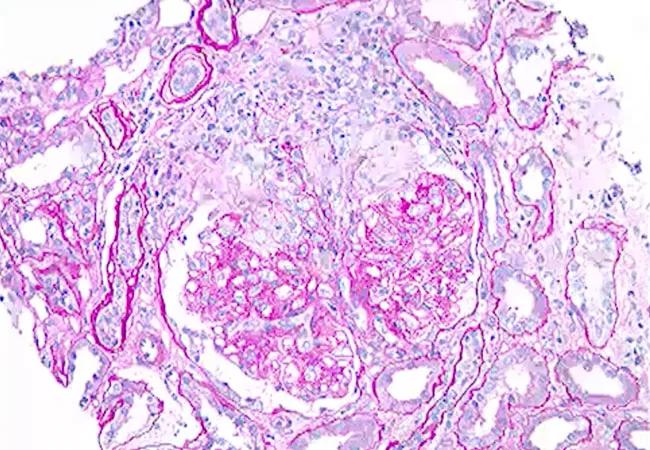
GPA and MPA are antineutrophil cytoplasmic autoantibody (ANCA)-associated vasculitides disorders, characterized by systemic autoimmune small-vessel vasculitis. While these disorders can involve vasculitis of any organ or tissue, the upper and lower respiratory tracts and the kidneys are most likely to be affected. GPA is often, but not always, associated with proteinase 3-ANCA, while MPA is more likely to be associated with myeloperoxidase-ANCA.
Although more common in adults, GPA and MPA also occur in children. Disease manifestations are similar in adult and pediatric patients, and the effects can be severe, even life-threatening.
The Pediatric Polyangiitis Rituximab Study (PePRS) included 25 pediatric patients with a median age of 14 across 11 centers. Patients had new or recurrent disease, 19 (76%) with GPA and six with MPA (24%).
During the initial six months of the remission-induction phase, patients received intravenous infusions of RTX (375 mg/m2 body surface area) once weekly for four weeks in addition to glucocorticoids (GCs). In the follow-up period, RTX or another immunosuppressant was administered at the discretion of the treating physician, and the safety and efficacy profile was further evaluated. Although the majority (68%) were followed from 18 months to three years, some patients (24%) were followed for three to 4.5 years.
The authors report that remission, as defined by the Pediatric Vasculitis Activity Score, was achieved in 56%, 93%, and 100% of patients by months six, 12 and 18, respectively.
Advertisement
Andrew Zeft, MD, an author of the study and Director of the Center for Pediatric Rheumatology at Cleveland Clinic, says these findings, which paved the way for the drug’s FDA approval in children for the treatment of GPA and MPA disease, validate what pediatric rheumatologists have generally experienced in their practice.
More than 10 years ago, findings from the Rituximab in ANCA-Associated Vasculitis (RAVE) trial evaluated the efficacy and safety of RTX as remission-induction treatment in adult patients with severe GPA or MPA. This led to the approval of RTX, in conjunction with GCs, as standard treatment for the diseases.
“There are good data in the adult setting, but these can’t always be extrapolated into a pediatric setting. However, given the rarity of the disease, the absence of treatment guidelines for pediatric GPA/MPA, and a similar pathogenesis in adults and children, the medication’s use for pediatric age GPA and MPA cases has been a carefully calculated decision in the appropriate clinical situation,” says Dr. Zeft.
“Fortunately, these data give us scientific evidence to guide future practice decisions, and not just reassuring clinical anecdotes.”
The authors report that the safety profile of RTX in pediatric patients with GPA or MPA was generally consistent with that of adult patients. However, a secondary analysis using data from the PePRS cohort aimed to assess the impact of longer-term safety associated with prolonged acquired immunodeficiency and risk for serious infection in pediatric patients following RTX treatment.
Advertisement
Though RTX, a B-cell-depleting therapy, can lead to hypogammaglobulinemia (HGG), the clinical significance of this was not known, the authors note. Some patients with HGG are seemingly unaffected, while others may experience recurrent or severe infection.
Findings show that the majority of pediatric GP and MPA patients did have prolonged low levels of immunoglobulin at month 18 of follow-up, including 18 patients (72%) with low immunoglobulin G, 19 patients (76%) with low immunoglobulin M, and 15 patients (60%) with both. However, altogether there were only nine serious infections reported in seven patients (28%). These events were all managed medically, and an increased number of infections did not occur with additional RTX treatments.
Dr. Zeft says since FDA approval of the drug, he suspects many more children with GPA or MPA are being managed with RTX. He is hopeful this will pave the way for a larger-scale patient registry and broader future study.
“Overall, we are pleased that the drug appears reasonably safe in pediatric patients, but we also believe future longitudinal assessments will help inform management of risk and infections associated with treatment of these specialized patients.”
Advertisement
Advertisement

Findings hold lessons for future pandemics

One pediatric urologist’s quest to improve the status quo

Overcoming barriers to implementing clinical trials

Interim results of RUBY study also indicate improved physical function and quality of life

Innovative hardware and AI algorithms aim to detect cardiovascular decline sooner

The benefits of this emerging surgical technology

Integrated care model reduces length of stay, improves outpatient pain management

A closer look at the impact on procedures and patient outcomes