
Routine lateral pelvic lymph node dissection for Stage III rectal cancer may not be warranted for all patients. Instead, a selective strategy focusing only on positive node disease following neo-adjuvant treatment could target those patients most likely to benefit, new research presented at Digestive Disease Week 2018 suggests.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Cleveland Clinic researchers studied 166 patients who underwent curative surgery for locally advanced rectal adenocarcinoma. Almost 30 percent had evidence of pelvic lymph node disease on preoperative MRI. The investigators compared their outcomes with the remaining 70 percent who did not have positive disease on imaging.
Before surgery, some patients underwent neoadjuvant chemoradiotherapy. More node-positive patients underwent chemoradiotherapy, 88 percent, compared to 70 percent of the node-negative group.
“Patients who had positive lymph nodes before radiation and chemotherapy had worse outcomes — their local recurrence-free survival was worse than patients who did not have any lymph node involvement in the pelvic area,” says Cleveland Clinic colorectal surgeon and study senior author I. Emre Gorgun, MD.
After a median follow-up of 46 months, a larger proportion of patients in the positive lateral pelvic node disease group experienced local recurrence rates of their cancer, 20 percent, versus 6 percent in the other group. This difference was statistically significant (P = 0.005). Overall survival (P = 0.46) was comparable and recurrence-free survival rates were significantly worse in the lateral node positive group (P = 0.01) on a Log-rank test.
“Based on that, we are concluding if patients have positive lateral pelvic lymph nodes before and after neo-adjuvant treatment, those patients’ may benefit from lateral pelvic lymph node dissection.”
Lead study author Ipek Sapci, MD, Cleveland Clinic colorectal surgery research fellow, presented the findings Sunday during a Small Bowel and Colorectal Plenary Session at the DDW gastroenterology conference in Washington, D.C.
Advertisement
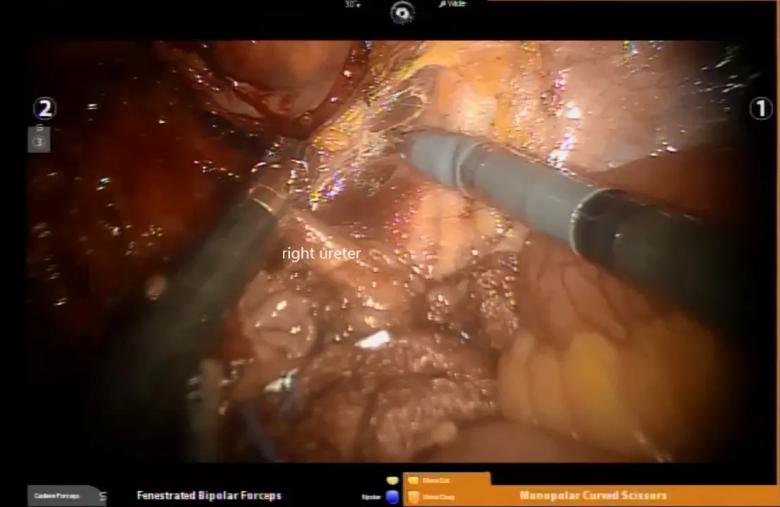
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/33a0c806-b989-49a1-8aa6-f7457df9e97b/LN-dissection_1_jpeg)
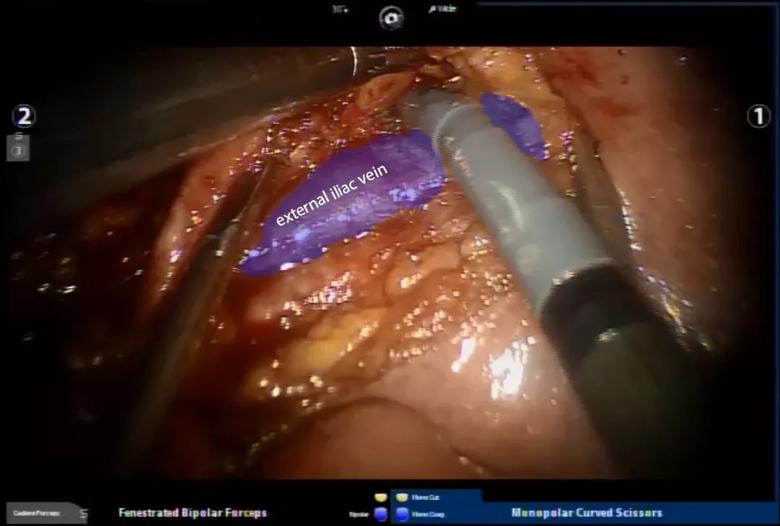
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/7303b19f-de90-47d1-8aa5-1e7e66d86ded/LN-dissection_2_ext_iliac_jpeg)
The study population had a mean age of 58 years and 72 percent were male. A total 49 patients had positive iliac or obturator pelvic node disease on preoperative imaging, according to data from a prospectively maintained database and additional chart reviews. Within this group, 17 patients also had a post-neoadjuvant treatment MRI. This imaging revealed a decrease in the size of nodes or resolution of nodal disease among 15 patients.
Optimal management of lateral pelvic nodal disease in locally advanced rectal cancer remains debatable around the world, the authors noted. In Japan, for example, this type of dissection is more common, even among rectal adenocarcinoma patients who do not have evidence of lateral pelvic lymph node involvement, Dr. Gorgun says.
“Japanese surgeons routinely perform lateral pelvic lymph node dissection. However, the data there is questionable,” Dr. Gorgun says. There is no clear evidence that, on ‘all comers,’ that taking out those lymph nodes provides benefit.”
Removing the nodes regardless of imaging evidence could expose some patients to longer surgeries and greater morbidity, he adds. “We are proposing a more selective approach in our dataset.”
Even though overall survival were not statistically significant, the finding of greater recurrence and worse recurrence-free survival among those with evidence of nodal disease warrants further study, Dr. Gorgun says. “Patients with this type of presentation [positive nodes on MRI] should not be ignored. This is an important aspect of rectal cancer that is often overlooked,” he says.
Advertisement
“These lymph nodes should be removed in the appropriate patients,” Dr. Gorgun explains. “Dissection of lymph nodes in that area is technically demanding; it’s close to vital structures like veins, the iliac artery and nerves. You really need good technical skills and dexterity.”
If a surgeon is not comfortable performing lateral pelvic lymph node dissection in patients with rectal cancer, they can refer them to a center with surgeons with specific expertise in this area. At Cleveland Clinic, for example, he says, “patient volume and ancillary staff like research fellows and personnel who are readily available for us allow us to do studies like this. Additionally, technologies such as robotics facilitates these technically demanding procedures accomplished with ease.”
Advertisement
Advertisement

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Potentially cost-effective addition to standard GERD management in post-transplant patients

Findings could help clinicians make more informed decisions about medication recommendations

Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care

Retrospective analysis looks at data from more than 5000 patients across 40 years

Surgical intervention linked to increased lifespan and reduced complications