Mild recurrent ileal inflammation is more prognostic of worsening disease
Mild ileal recurrence of Crohn’s disease (CD) following ileocolonic resection — but not the presence of isolated anastomotic lesions — appears to drive the risk of progression to severe endoscopic disease, Cleveland Clinic researchers have found.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The discovery of a predictive association between the postoperative development of mild inflammation in the small bowel and severe progression, and the lack of a similar association involving isolated anastomotic lesions, resulted from a retrospective cohort study of adult CD patients. The research was by gastroenterologist Benjamin Click, MD, and colleagues including Salam Bachour, a fifth-year medical student at Cleveland Clinic Lerner College of Medicine. Their findings were presented at the American College of Gastroenterology’s 2021 annual scientific meeting.
The study’s results help inform an ongoing debate regarding the prognostic significance of various signs of inflammation observed during postresection endoscopic monitoring. There has been disagreement about the clinical import of isolated aphthous, or erupted, inflammatory lesions at the ileocolonic anastomosis site, compared to inflammation elsewhere in the small bowel.
“Historically, we attributed anastomotic lesions to ischemia resulting from resection,” Dr. Click says. “More and more, we’re understanding that these ulcerations at the anastomosis are Crohn’s disease. But the question then becomes do these isolated lesions convey a risk of disease progression? There’s been conflicting data in the literature about this.”
Although medical management of CD has improved over time, as many as two-thirds of patients eventually require surgical intervention such as bowel resection and anastomosis to address symptoms, resolve complications and improve quality of life.
Advertisement
Unfortunately, CD recurs postoperatively at the neoterminal ileum in 30% to 90% of patients within a year of surgery, and almost universally within five years. The likelihood of recurrence appears higher following ileocolonic resection and anastomosis.
Endoscopic examination is the clinical standard for assessing CD status and progression and enables detection of presymptomatic CD recurrence.
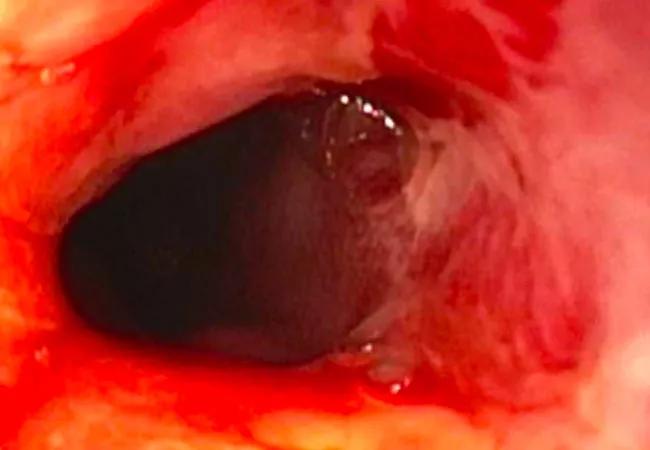
Used in conjunction with ileocolonoscopy, the Rutgeerts score is a grading system developed to predict clinical CD recurrence in patients who have undergone ileocolonic resection and anastomosis. A CD patient’s Rutgeerts grade is based on the observed number and size of aphthous lesions in the neoterminal ileum and the characterization of the mucosa between the lesions. Rutgeerts grades range from i0 (no lesions) to i4 (diffuse mucosal inflammation with more than 5 large ulcers and/or nodules and/or stenosis).
The severity of endoscopic recurrence as graded by the Rutgeerts score is intended to predict clinical outcomes, with scores of i2 or higher representing an increased risk of symptomatic recurrence. However, there is currently no formal validation of the Rutgeerts score.
The middle Rutgeerts category, i2, has been the subject of disagreement because its original description incorporated both mild inflammation in the distal ileum and at the anastomosis site, with heterogeneous recurrence risk. “There’s been debate in the literature about whether there is a differential risk of disease recurrence related to the location of inflammation within that category,” Dr. Click says.
Advertisement
The i2 category subsequently was modified into two subdivisions: i2a (isolated lesions confined to the anastomosis) and i2b (more than five aphthous ulcers in the neoterminal ileum, with or without anastomotic lesions).
The change did not resolve questions about the prognostic significance of either subdivision’s inflammatory features. A retrospective study published in 2019, for example, found no difference in clinical recurrence and need for endoscopic or surgical intervention between patients with i2a or i2b endoscopic recurrence. Conversely, a 2020 retrospective study in which Cleveland Clinic researchers participated found that anastomotic ulcers independently predicted disease progression.
In the latest research, Dr. Click says, “we sought to compare the difference in future endoscopic recurrence risk, or progression to more severe recurrence, between these two subcategories.”
The researchers retrospectively evaluated the postoperative disease course of 199 adult CD patients who had undergone ileocolonic resection between 2009 and 2020 at Cleveland Clinic. The cohort included patients with bowel continuity restoration, an index postoperative ileocolonoscopy within 18 months of surgery graded at between i0 and i2b on the modified Rutgeerts scale, and one or more subsequent colonoscopies.
In cases where there was no prospective Rutgeerts score in a patient’s medical record characterizing their ongoing disease status, a centralized reader retrospectively assigned one by reviewing clinical text and endoscopy images, Bachour says. The reader was trained and validated on a dataset that was not included in the study database.
Advertisement
The study’s primary outcome was severe endoscopic progression, defined as either i3 or i4 disease. The secondary outcome was surgical recurrence, defined as repeat ileocolonic resection.
Overall, 26% of patients experienced severe endoscopic CD progression. Using multivariate analysis and adjusting for risk factors (tobacco use, more than two prior ileocolonic resections and/or use of biologics after the index ileocolonoscopy), i2b disease was found to be associated with decreased time to severe endoscopic CD progression compared to i0, i1 (p<0.001) or i2a (p=0.002) disease. Conversely, i2a disease — meaning isolated anastomotic lesions — was not associated with decreased time to severe endoscopic CD progression compared to i0 or i1 disease (p=0.25).
Dr. Click notes that the prognostic association between i2b disease and severe endoscopic CD progression was consistent whether the i2b grade was based on the index postoperative ileocolonoscopy or a subsequent one. “The association held at both time points,” he says.
Surgical recurrence, meaning a patient’s need for repeat ileocolonic resection, was not associated with the patient’s index Rutgeerts score (p=0.86), the study found.
21-DDI-2370210The study’s conclusion is that the risk of progression to severe endoscopic activity appears to be driven by ileal inflammatory involvement rather than isolated anastomotic inflammation, Bachour says.
The presence of isolated anastomotic ulcers “conveys a reduced risk, at least in our single-center data set, and that has been confirmed by others as well,” Dr. Click adds. “However, it doesn’t mean that patients with i2a disease are risk-free. Both sets of individuals — in categories i2a and i2b — need ongoing monitoring and surveillance for disease recurrence. But perhaps those with ileal involvement are a higher-risk subgroup and may need to be followed more closely, with possible modifications to their medical therapy regimen as a result.”
Advertisement
Another finding with potential clinical significance: Starting biological therapy when an ileocolonoscopy reveals i2b inflammation is associated with a reduced risk of disease progression. “An important takeaway from the study is that those patients with mild ileal inflammation, if they are not on a biologic at the time of that finding, may benefit from the initiation of such,” Dr. Click says.
The study did not identify an association between smoking or multiple prior ileocolonic resections and severe endoscopic CD progression. Previous research had suggested those were risk factors.
Prospective studies with larger cohorts are needed to validate the retrospective study’s findings and to help further quantify and explain the impact of mild ileal recurrence on severe CD progression.
“Whenever dealing with retrospective data and smaller sample sizes, those have to be taken into consideration as a potential limitation,” Dr. Click says. “But otherwise, I think these findings are in line with our clinical experience and provide us more data to help guide risk stratification in this important patient population.”
Advertisement

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Potentially cost-effective addition to standard GERD management in post-transplant patients

Findings could help clinicians make more informed decisions about medication recommendations

Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care

Retrospective analysis looks at data from more than 5000 patients across 40 years

Surgical intervention linked to increased lifespan and reduced complications