Too few patients assessed before undergoing biologic dose changes
Clinicians do not administer reactive therapeutic monitoring (TDM) or objective disease activity assessments prior to making changes in biologic therapies in almost a third of patients with inflammatory bowel disease (IBD). So finds an analysis of objective marker and TDM assessments used routinely in clinical practice when patients do not respond to biologic therapies, recently published in Gastroenterology.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Current IBD treatment standards recommend that clinicians perform reactive TDM and objective disease activity assessment before changing a patient’s biologics. “The current guidelines recommend that patients who are on biologics but have active disease receive TDM and objective assessments,” says Benjamin Click, MD, MS, first author of the study and Cleveland Clinic gastroenterologist. “We wanted to evaluate the real-world implementation of these recommendations.”
Over 2100 patients with IBD were enrolled in this prospective, longitudinal, multisite study between June 2017 and October 2019. Patients were on biologic therapy and had either a dose change or discontinuation due to a perceived lack of efficacy. Clinicians obtained fecal calprotectin, CRP, endoscopy or cross-sectional imaging on all patients within 12 weeks prior to the changes, and TDM data for infliximab and adalimumab were obtained. Patients who had undergone surgery within three months were excluded, and only the first therapeutic change was evaluated.
Of the larger cohort, 537 patients had a dose change in (55.9%) or discontinued (44.1%) biologic therapy for lack of efficacy. Of these patients, most were female (58.1%), Caucasian (85.7%) and between 18-39 years old (52.5%). Seventy-one percent of patients had Crohn’s disease (CD), and 28.7% had ulcerative colitis (UC).
“We found that a little over two-thirds [68%] of patients seeking a dose change had at least TDM or objective disease activity assessment,” says Dr. Click. “When the guideline is for all patients seeking a dose change or continuation, and the majority were seen at an academic medical center, this number is too low.” For patients who discontinued biologics, the number who received assessment or TDM was slightly higher at 71.7%. Multivariate regression analysis did not reveal any characteristics of patients or their disease associated with TDM or objective assessment.
Advertisement
Researchers also found that types of testing differed by disease. For patients seeking dose change, CRP was the most common objective marker used in both CD and UC, but CRP and calprotectin were both used significantly more in patients with UC (P = 0.007). Patients with UC received more CT (P = 0.05). TDM was only ordered in about 20% of patients regardless of disease type. Patients with CD being evaluated for discontinuation had CT (P = 0.04) and MRI (P = 0.002) more frequently than those with UC. Patients with UC received endoscopy more commonly (P = 0.01).
Now that the landscape of testing is understood, Dr. Click says the next step is to find out why. “We need an improved understanding of why we fall short in objective assessments and instead empirically change or discontinue therapy,” he says. “Discerning the why may help us optimize biologic treatments and outcome for patients with Crohn’s and ulcerative colitis.”
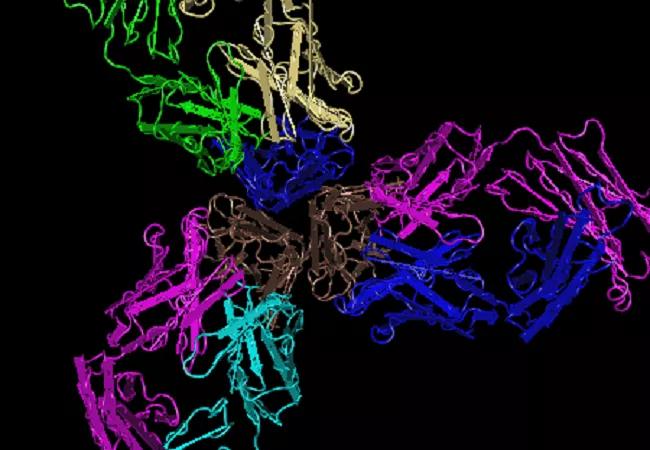
Image: 3D molecular image of the crystal structure of TNFα in complex with the anti-TNF agent infliximab Credit: National Center for Biotechnology Information.
Advertisement
Advertisement

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Potentially cost-effective addition to standard GERD management in post-transplant patients

Findings could help clinicians make more informed decisions about medication recommendations

Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care

Retrospective analysis looks at data from more than 5000 patients across 40 years

Surgical intervention linked to increased lifespan and reduced complications