An effective, patient-centered biospy alternative
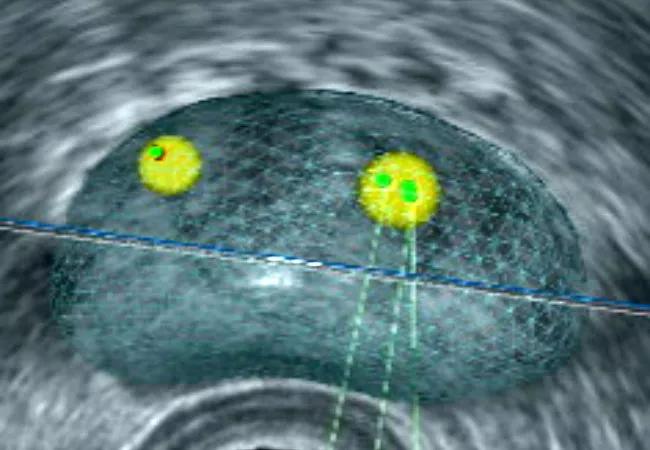
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/bc92518a-b08d-4a7c-b25b-850d91b45d0c/650x450-Klein_jpg)
Transperineal Fusion-Guided Biopsy
Improved imaging technology and a shift in diagnostic practice are making transperineal fusion-guided biopsy a popular approach among urologists at Cleveland Clinic.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In fact, Zeyad Schwen, MD, urologic oncologist in the Glickman Urological & Kidney Institute, predicts this biopsy technique will become the new gold standard. “It’s more accurate and more comfortable for patients, plus there is a lower risk of infection and rectal bleeding,” he says.
Transrectal ultrasound (TRUS) prostate biopsy has been a mainstay for decades, but it’s not without risk. Because the prostate is accessed via the rectal wall, there is a greater potential for bacterial infection, and it can be painful for some patients. Further, biopsy obtained through the rectum can result in undersampling, particularly in the anterior prostate, according to some studies.
As for transperineal biopsy, the urologist guides the biopsy needle through perineal skin and into the prostate, as opposed to the rectal wall. Though the ultrasound is still placed in the rectum, the risk for developing an infection and for rectal bleeding decreases considerably, explains Dr. Schwen. It can be performed with local anesthesia, similar to a traditional biopsy, or under sedation, and patients tend to report a better experience, he says.
This approach is particularly well-suited for patients who have a history of infection or sepsis following transrectal biopsy or those at risk for bacteremia-induced complications (e.g. patients with a heart valve or vascular graft).
Several years ago, urologists at Cleveland Clinic began incorporating multiparametric magnetic resonance imaging (MP-MRI) techniques to complement TRUS. MP-MRI enabled them to apply a richer layer of information to better localize and characterize prostate cancer lesions.
Advertisement
This was soon followed by MRI/TRUS fusion-guided biopsy, a technology that fuses MRI images with ultrasound images taken during the biopsy. This allows the physician to target any concerning areas from the MRI in real-time. Now, this technique is being applied to transperineal approaches. While MRI-based technology has been the norm, the team also recently added a micro-ultrasound imaging modality to their diagnostic toolkit, one that may eventually replace the need for MRI, allowing imaging and biopsy to be completed in one setting.
Findings from a recent study conducted outside of Cleveland Clinic show no meaningful difference between the use of transrectal or transperineal approaches when it comes to detecting clinically significant prostate cancer.
Dr. Schwen says that this news should be encouraging to those who have recently – or are considering – implementing this biopsy technique into their practice. “It’s a safe and effective alternative and, importantly, patients are reporting higher levels of satisfaction.”
Advertisement
Advertisement
Pediatric urologists lead quality improvement initiative, author systemwide guideline
Fixed-dose single-pill combinations and future therapies
Reproductive urologists publish a contemporary review to guide practice
Two recent cases show favorable pain and cosmesis outcomes
Meta-analysis assesses outcomes in adolescent age vs. mid-adulthood
Proteinuria reduction remains the most important treatment target.
IgA nephropathy is a relatively common autoimmune glomerular disease that can be diagnosed only by biopsy
Oncologic and functional outcomes are promising, but selection is key