Expert insights from a milestone congenital heart surgery study
Since the first publication of results from the Single Ventricle Reconstruction (SVR) trial in 2010 (N Engl J Med. 2010;362:1980-1992), this landmark randomized investigation has yielded 83 post hoc study publications, including the much-anticipated SVR Extension Study (SVR II) by Newburger and colleagues last year (Circulation. 2018;137:2246-2253).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
This collective research output led the editors of the Journal of Thoracic and Cardiovascular Surgery to deem the SVR trial one of the most important congenital heart surgery studies of the past decade. It also prompted them to invite a team of expert congenital heart surgeons, led by Cleveland Clinic’s Tara Karamlou, MD, MSc, to analyze and contextualize the findings of SVR II in an expert opinion feature (J Thorac Cardiovasc Surg. 2019 Apr 17 [Epub ahead of print]). This article summarizes six key takeaways from that editorial after recapping the SVR II essentials.
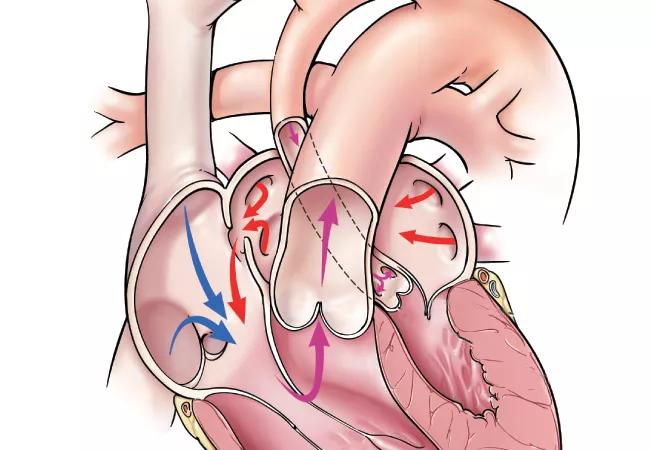
SVR II set out to compare transplant-free survival and other outcomes among 549 children with hypoplastic left heart syndrome (HLHS) enrolled in the SVR trial after the last enrollee had reached age 6 years. Patients had been randomized as neonates to undergo the Norwood procedure with either the Sano right-ventricle-to-pulmonary-artery shunt (RVPAS) or a modified Blalock-Taussig shunt. One-year results, as reported in the initial SVR report in 2010, had shown superior one-year transplant-free survival in the RVPAS group versus the Blalock-Taussig shunt group.
In SVR II, three time intervals were studied: before stage II surgery, between stage II surgery and the Fontan procedure, and after the Fontan procedure. Key findings of SVR II included the following:
Advertisement
Findings resonate with other recent multicenter data. In their editorial, Karamlou and colleagues call the SVR II findings “sobering” in view of the modest transplant-free survival rates at mid-term follow-up after Norwood reconstruction. They note that while some single-center reports have raised hopes that better outcomes are achievable, recent multicenter reports are consistent with the SVR II outcomes. These include the Society of Thoracic Surgeons’ Congenital Heart Surgery Database 2018 annual report, the latest update from the Pediatric Heart Network-sponsored Fontan cross-sectional cohort, and the latest data from a Congenital Heart Surgeons’ Society cohort of post-Norwood infants.
“The more optimistic findings from single-institution series need to be viewed with circumspection,” says Dr. Karamlou. “As for many complex problems where there is considerable data variance, the devil is in the details.”
It may be time to make overall survival a primary outcome. Use of transplant-free survival as the primary outcome metric in SVR II may carry important limitations over longer-term follow-up, the editorialists contend. They note that overall survival may be a more meaningful measure in the setting of single-ventricle palliation, as heart transplantation is increasingly an inevitable step in such palliation — and one that tends to improve health-related quality of life and functional status.
There’s even a case to be made from a cost perspective, the editorialists write: “[A]n equitable comparison of the overall care burden should include transplantation compared with the chronic care pathway experienced by patients with suboptimal single-ventricle physiology.”
Advertisement
“Adding overall survival as a primary outcome as the SVR cohort matures may yield important data to inform whether and when to triage patients to transplantation,” Dr. Karamlou observes.
Practice standardization is imperative. SVR II’s demonstration that shunt type has limited influence on outcomes raises the question of whether other, more comprehensive strategies that encompass the entire patient experience should be pursued to improve outcomes in HLHS. The editorialists write that the “tremendous variability in practices” seen in the SVR trial offers a promising opportunity in this regard. Examples of that variability abound: Across the 15 SVR trial sites, rates of delayed sternal closure ranged from 35% to 100%, extubation within 72 hours of Norwood varied from 5% to 63%, and discharge on all-oral feeds ranged from 3% to 81%.
“A main impediment to development of best practices in the care of the Norwood population is a lack of standardized definitions for important complications, such as arch obstruction,” says Hani Najm, MD, Chair of Pediatric and Congenital Heart Surgery at Cleveland Clinic and another co-author of the editorial. “This confounds our ability to consistently study outcomes across centers and establish useful performance benchmarks.”
To that end, the editorialists call for establishment of a range of acceptable criteria for intervention and structured implementation of protocols derived from high-performing centers, with the aim of reducing variation and improving outcomes.
Advertisement
Regionalization is easier said than done. Citing case volume-based survival benefits, Karamlou and colleagues recognize that regionalization of care is another promising pathway toward improved outcomes in the setting of HLHS. “A regionalized care system has clear appeal,” says Dr. Karamlou, “but its implementation poses many challenges.” Key among them, she notes, is the need to adjudicate appropriate measures for designating centers of excellence and a need for considerable scalability of resources, infrastructure and personnel.
Alternative initial therapy has a role. The editorialists note that alternatives to the Norwood operation, including primary transplantation or hybrid palliation combining catheter intervention with surgery, have shown promise when applied judiciously to appropriate candidates. “Excellent long-term outcomes in populations with HLHS will likely require the ability to integrate empiric best practices learned from other groups with experience in these alternatives,” Dr. Najm observes.
Comprehensive longitudinal surveillance is essential. The SVR trial sites with better long-term survival rates share “a focused commitment to iteratively implement changes based on comprehensive analyses of the current longitudinal care paradigm,” the editorialists write. They cite the example of how a 2003 publication on the potential benefits of interstage post-Norwood home-monitoring programs (J Thorac Cardiovasc Surg. 2003;126:1367-1377) led to widespread adoption of similar programs through a collaborative initiative, with broad subsequent reductions in interstage mortality.
Advertisement
“This type of harmonizing of avenues of research and practice among multiple centers will be essential to overcoming the many remaining unknowns in the long-term management of children with HLHS,” says Dr. Karamlou. “The more such collaboration goes beyond mortality and morbidity to reflect a comprehensive approach to care, the more these children will thrive.”
The full expert opinion piece is available here.
Advertisement

Scenarios where experience-based management nuance can matter most

Introducing Krishna Aragam, MD, head of new integrated clinical and research programs in cardiovascular genomics

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients