Three criteria for finding an effective treatment for neurodegeneration
The phase 2b Multiple Sclerosis-Secondary Progressive Multi-Arm Randomisation Trial (MS-SMART) was thought to be the next best hope for finding a drug therapy to slow neurodegeneration, but it has proved to be another dead end for people with progressive multiple sclerosis (MS). So report the study’s investigators in a new article published online by The Lancet Neurology.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Amiloride, fluoxetine and riluzole — the three drugs chosen to be tested for neuroprotection — showed the best potential of more than 500 candidate test drugs screened in a systematic review. Nearly 450 patients were randomly assigned treatment with one of these three drugs or placebo over 96 weeks. An impressive 88% of patients completed the study. However, the well-designed, well-executed trial didn’t produce the much-anticipated result: reducing percentage brain volume change as detected by MRI. None of the test drugs performed better than placebo.
Robert Fox, MD, a neurologist with Cleveland Clinic’s Mellen Center for Multiple Sclerosis Treatment and Research, reflected on this outcome in an invited commentary that accompanies the MS-SMART report in The Lancet Neurology.
“These disappointing results raise an obvious question: Why was a promising treatment not identified to carry forward into phase 3 trials?” he writes.
Dr. Fox goes on to offer three possible explanations that correspond with possible modifications for future studies. To ultimately identify an effective therapeutic for progressive MS, he says, researchers first must:
Advertisement
“The negative outcome of MS-SMART, and many other trials in neurodegenerative diseases, points to an urgent need to rethink how we select and test experimental treatments for neurodegenerative conditions,” writes Dr. Fox.
Fortunately, MS-SMART also incidentally shows ways for neurology researchers to redirect their efforts. Hitting a dead end just signals another turn on our continuing journey toward an effective therapeutic for progressive MS.
Read Dr. Fox’s full commentary here. For more insights on this topic from Dr. Fox, check out the below episode of Cleveland Clinic’s Neuro Pathways podcast for healthcare professionals.
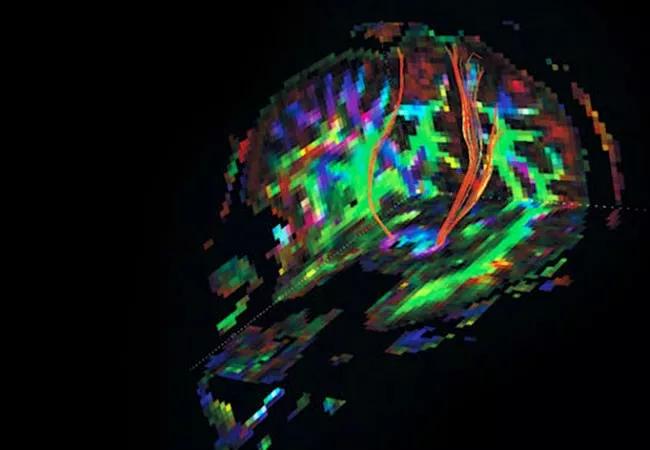
Image at top shows corticospinal tracts from a diffusion tensor imaging study from a patient with progressive MS.
Advertisement
Advertisement

Aim is for use with clinician oversight to make screening safer and more efficient

Rapid innovation is shaping the deep brain stimulation landscape

Study shows short-term behavioral training can yield objective and subjective gains

How we’re efficiently educating patients and care partners about treatment goals, logistics, risks and benefits

An expert’s take on evolving challenges, treatments and responsibilities through early adulthood

Comorbidities and medical complexity underlie far more deaths than SUDEP does

Novel Cleveland Clinic project is fueled by a $1 million NIH grant

Tool helps patients understand when to ask for help