Patients with early failure of total hip arthroplasty have worse function after revision than patients with later failure

Patients who undergo aseptic revisions of total hip arthroplasty (THA) soon after the primary procedure report worse outcomes than those whose revisions occur later. However, there appears to be little difference in rates of readmission or death between the two groups.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Those were among the findings of an analysis of data from 572 patients who had THA followed by aseptic revision at Cleveland Clinic from August 2015 to December 2018. The 176 patients with aseptic failures occurring in under three years were compared with 396 patients whose failures occurred in three years or later.
“We wanted to understand if the overall outcome in terms of pain and function was different when we had to take a patient back early on, compared to doing the revision later. We wanted to have some sort of guidance for patients,” says senior author Carlos A. Higuera, MD, Chair of the Levitetz Department of Orthopaedic Surgery at Cleveland Clinic Weston Hospital.
This issue is becoming more important as the number of total hip replacements in the U.S. continues to rise. One study estimates more than 1 million total hip replacements per year by 2040.
The need for revision — currently about 4%-5% within three years and about 8%-10% beyond — has dropped over time thanks to improvements in materials and techniques. Moreover, “we optimize patients more for the procedure, so we decrease the risk of complications,” says Dr. Higuera.
However, because the number of hip replacements is increasing so dramatically, the overall number of implant failures has either stayed the same or increased.
“In the past, probably the No. 1 reason for revision was aseptic loosening and wear, since the materials weren’t as good as they are today,” explains Dr. Higuera. “That reason has almost disappeared. Today, the main reason is infection. We’re more concerned about that because we can’t do much to control it other than optimize risk factors such as smoking, obesity, diabetes and immunosuppression. Thankfully, the rate of infection is not that high — about 1%-2% for all primary joints.”
Advertisement
The recent study by Dr. Higuera and colleagues was limited to aseptic revisions.
In the study, most of the early revisions were for bone-related diagnoses (22.7% versus 8.3% of late revisions) or other complications (19.9% versus 5.8%). More late revisions were due to implant failures (37.1% versus 6.8%). Rates of instability and aseptic loosening were similar between the groups.
Operative time was shorter in early revisions when compared to late revisions (133 minutes versus 157 minutes). However, there were no significant differences between the groups in use of cemented versus uncemented fixation types, use of acetabular fixation materials, length of stay, discharge disposition, 90-day readmission, re-revisions or one-year mortality.
Preoperatively, scores on patient-reported outcome measures (PROMs) of pain and physical function were worse in the early revision group. While these scores improved at one year after revision (including with a significantly higher delta change in physical function), they still were worse than the late revision group’s one-year postoperative scores.
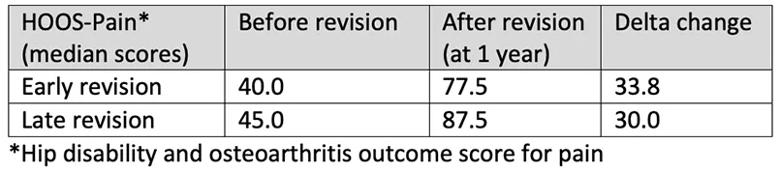
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/6a6c5500-1319-479b-a37d-993dc11dce6b/23-ORI-4208958-CQD-Table1_jpg)
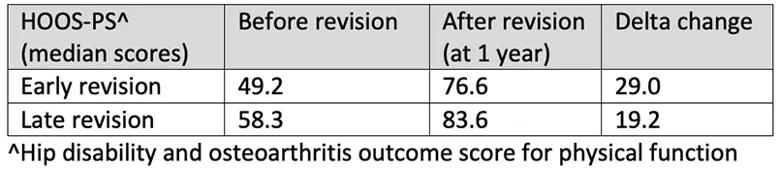
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/692920b6-ae90-4e8e-a003-48eab23bc310/23-ORI-4208958-CQD-Table2_jpg)
After adjustment for multiple confounding variables, patients who had revision because of aseptic loosening were significantly more likely to improve than were those who had revision due to implant failure (odds ratio [OR] 0.29, P < .001). Similarly, those whose revisions were due to instability had fewer treatment failures compared to those who had revision due to implant failure (OR 0.28, P = .02).
Advertisement
These data highlight the importance of making every effort to optimize the initial THA procedure, says Dr. Higuera. Revisions, when needed, should be performed by experienced surgeons at high-volume centers.
“A review of the literature shows that when revisions are done in high-volume centers, the overall complication rate is lower, and later pain and function are improved,” he says.
Three major advances have helped reduce total joint revision rates at Cleveland Clinic, he adds:
“All of this, combined with optimization of patients, decreases the number of total joint failures,” says Dr. Higuera.
For more information, visit Cleveland Clinic Florida ConsultQD. Subscribe to the Florida Physician Newsletter.
Additionally, follow us on X (formerly Twitter), Facebook, and LinkedIn.
Advertisement
Advertisement

Nonthermal technique reduces bleeding and perforation risk

Standardizing a minimally invasive approach for Barrett’s Esophagus and Esophageal Cancer

PSMA-targeted therapy for metastatic prostate cancer now offered at Cleveland Clinic Weston Hospital

Nationally recognized urologic oncologist offers vision for growth, innovation, and excellence

Noninvasive modality gains ground in United States for patients with early-to-moderate disease

Cleveland Clinic Weston Hospital’s collaborative model elevates care for complex lung diseases

Interventional pulmonologists at Cleveland Clinic Indian River Hospital use robotic technology to reach small peripheral lung nodules

Trained in the use of multiple focal therapies for prostate cancer, Dr. Jamil Syed recommends HIFU for certain patients with intermediate-risk prostate cancer, especially individuals with small, well-defined tumors localized to the lateral and posterior regions of the gland.