Multidisciplinary team of plastic surgeons and neurosurgeons correct severe, complex head deformity
The vast majority of babies with macrocephaly grow into their heads, but in the case of a child born with severe hydrocephalus and extreme macrocephaly that prevented turning, sitting or lifting the head, the result was a fluid-filled, severely dysmorphic posterior cranial vault that interfered with mobility and development. In this instance, a reduction cranioplasty with sub-total cranial vault remodeling was selected as the treatment option.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“We felt it would be beneficial to bring her head shape within normal limits for a child her age to improve her mobility, remove the excess subdural fluid and provide room for brain growth,” says Cleveland Clinic Children’s pediatric neurosurgeon Violette Recinos, MD.
Pediatric craniofacial surgeons Bahar Bassiri Gharb, MD, PhD, and Antonio Rampazzo, MD, PhD, joined Dr. Recinos in the 10-hour surgery performed on the patient’s first birthday. It was a severe case with many challenges, including prior placement of two shunts, the presence of a subdural hygroma and dramatically shifted anatomy caused by a significantly dysmorphic cranial shape.
The surgery achieved its goals, and eight weeks later, the child was able to lift her head. Now, after three years of weekly physical, occupational and speech therapy, her brain has grown, and she is catching up developmentally with other children her age.
“We are extremely gratified to see significant progress in her physical, emotional and cognitive development, along with significant radiographic changes,” says Dr. Recinos.
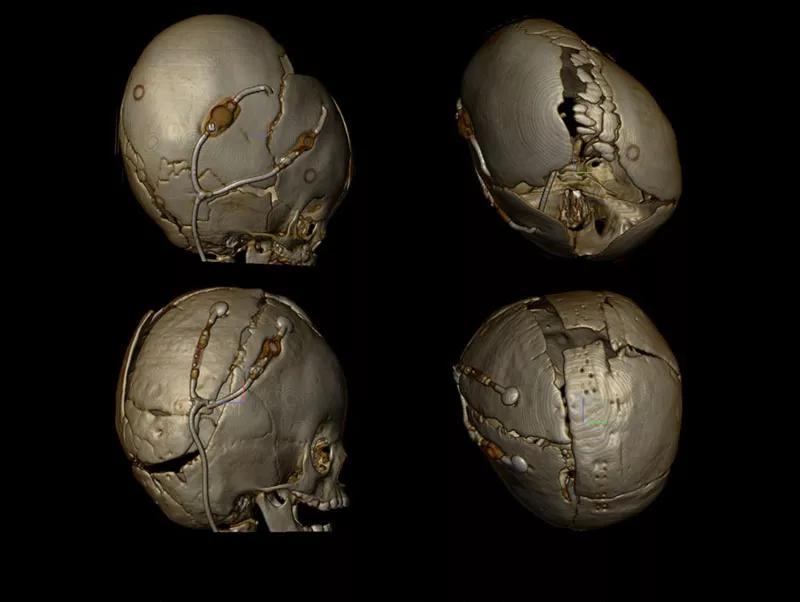
Massive in utero hydrocephaly that first required VP shunt and subduroperitoneal shunt because of sudural hygroma.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/867ef270-2305-4e7e-a1bb-d0a18883b9dd/19-PSX-6049-kaylee-scanHeadPre-800x602-150x113-jpg)
Patient was born with head circumference of 46cm.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/4710377c-c098-4def-8ba9-21c3f344f90e/19-PSX-6049-kaylee-newborn-800x602-150x113_jpg)
The parietal subdural shunt was removed during cranial vault remodeling, and a new shunt was placed after the bones were remodeled, repositioned and fixed.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/6dc219d5-fdf9-4769-8fd8-3040287d5b7d/19-PSX-6049-kaylee-skull6-800x602-1-150x113_jpg)
Pre-op, front view, October 2015. At 12 months, the patient presented with macrocephaly, positional plagiocephaly and was unable to hold her head up.
Advertisement

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/9bb4cf97-781a-4bfa-b378-3dd9cf12bf97/19-PSX-6049-kaylee-preOpFront-800x602-150x113_jpg)
Post-op, front view, August 2016.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a3c2383f-b4a7-4b7f-9b69-b08536088b62/19-PSX-6049-kaylee-postSurgVisitFront-800x602-150x113_jpg)
Pre-op, side view, October 2015.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/2cac3e83-e8c7-4bf7-9c95-1e0be36ba77e/19-PSX-6049-kaylee-preOpSide-800x602-150x113_jpg)
Post-op, side view, August 2016.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/7ef89ce7-ade1-48a2-9688-c08a994273d2/19-PSX-6049-kaylee-postSurgVisitSide-800x602-150x113_jpg)
Pre-op, top view, October 2015.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/120c963a-8f3e-4553-83c2-a33a3a6934be/19-PSX-6049-kaylee-preOpTop-800x602-150x113_jpg)
Post-op, top view, August 2016.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/6539c18f-3d55-4879-983e-bf78d52eff16/19-PSX-6049-kaylee-postSurgVisitTop-800x602-150x113_jpg)
Patient with Cleveland Clinic caregiver in 2018.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/fc2259b6-e841-4070-935b-fe9624b3ec4e/19-PSX-6049-kaylee-visitPostLongHr-800x602-150x113_jpg)
Slide 1/10
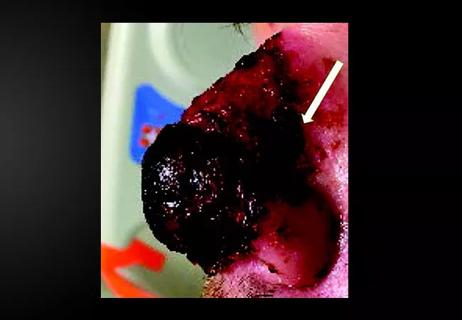
The patient was a 12-month-old female who was diagnosed in utero with massive hydrocephalus. At birth, her head measured 46 centimeters in circumference and comprised 5 pounds of her 7-pound total body weight.
The day after birth, a right ventriculoperitoneal shunt was placed. Three months later, she required a second shunt to drain a large subdural hygroma. Due to her massive head size, the child had limited mobility, and she developed severe left-sided positional plagiocephaly with a severely dysmorphic posterior cranial vault.
Further complicating this condition was a persistent large subdural collection, thought to be related to the excess skull space, which was interfering with brain growth. It became apparent that cranial vault remodeling would bring the head shape within normal limits and improve the child’s mobility. After the risks and benefits of this surgery were discussed in detail, the child’s parents agreed to the procedure.
Dr. Bassiri Gharb began by making a bicoronal incision to expose the patient’s entire cranial vault and shunt system. “Due to very significant left-sided flattening with subsequent right posterior bulging, the cranial shape was so significantly dysmorphic that normal landmarks—important structures—were not where they should have been,” says Dr. Bassiri Gharb. “We decided to make a small opening in the dura to drain excess spinal fluid and visualize the contour of the brain. This helped us to understand her anatomy, and prevent damage the sagittal sinus or other conduit that would have resulted in excess blood loss,” adds Dr. Recinos.
Advertisement
The dura was closed, and left and right craniotomies performed, working around the shunts. Dr. Recinos dissected the bone flaps in three large pieces, which Drs. Bassiri Gharb and Rampazzo used to model the skull shape. Bone was remodeled to correct the areas of flattening and prominence of the posterior skull base. The pieces of bone were reunited to complete the left skull, followed by the right skull, and reattached. New drill holes were placed and the shunts reattached and secured. The skin was re-draped to confirm satisfactory correction and the redundant skin and old scar tissue were removed. The patient was sent to the Pediatric Intensive Care Unit, where her recovery was uneventful.
Although the vast majority of children born with macrocephaly do not require cranial vault remodeling for cranial reduction, this procedure should be considered in severe cases.
“This is not a surgery to take lightly, since it can cause severe blood loss or other serious complication, including death on the operating table. It requires careful planning by a team of experienced surgeons,” says Dr. Bassiri Gharb. “That being said, this child looks great and is making terrific progress. I don’t foresee her needing more surgery to address head shape.”
Advertisement
Advertisement

Family history may eclipse sun exposure in some cases

Consider secondary syphilis in the differential of annular lesions

Persistent rectal pain leads to diffuse pustules

Two cases — both tremendously different in their level of complexity — illustrate the core principles of nasal reconstruction
Stress and immunosuppression can trigger reactivation of latent virus

Low-dose, monitored prescription therapy demonstrates success

Antioxidants, barrier-enhancing agents can improve thinning hair