A colorectal surgeon discusses the new care path
Thanks to recent advances, the multidisciplinary colorectal cancer team at Cleveland Clinic recently implemented a new care path that allows about a third of stage II and III patients to avoid surgery. ConsultQD spoke with David Liska, MD, Cleveland Clinic colorectal surgeon and Director of the Colorectal Cancer Multidisciplinary Tumor Board, whose research focuses on optimizing neoadjuvant treatment in locally advanced rectal cancer (LARC), about the new approach and its impact on patients.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Dr. Liska: The standard treatment used to involve several weeks of chemoradiation, followed by surgery, usually with temporary loop ileostomy, an additional four months of adjuvant chemotherapy, and then loop closure and surveillance.
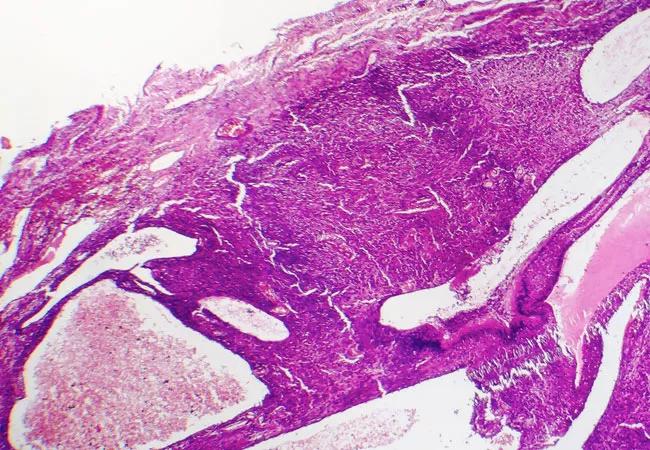
With this approach, histologic assessment showed that neoadjuvant chemoradiotherapy had induced a complete pathologic response in about 20 to 25% of patients. Theoretically, we could spare some patients major surgery. However, due to difficulty predicting a complete response (CR) before surgery and the potential risk for delayed recurrence, surgery was still recommended for everyone.
For about 18 months now, we have followed the protocol from the Organ Preservation in Rectal Adenocarcinoma [OPRA] trial, in which we participated. Patients diagnosed with stage II or III rectal cancer now receive total neoadjuvant therapy [TNT] up front, usually five weeks of chemoradiotherapy followed by four months of consolidation chemotherapy. If we see a CR on multimodal assessment following TNT, we implement active surveillance, which involves physical exam, flexible sigmoidoscopy, carcinoembryonic antigen levels and MRI and CAT scans at regular intervals for at least five years. About 30 percent of our patients can avoid surgery with this approach.
Dr. Liska: Some studies have shown that TNT results in higher CR rates. Other studies have shown that TNT facilitates complete delivery of planned systemic therapy. Furthermore, it usually results in patients needing less time with a diverting ileostomy. Importantly, this approach has been shown to have a higher CR rate, which provides the potential for organ preservation and active surveillance. Active surveillance has tremendous advantages for patients given the significant morbidity and quality of life implications associated with surgery.
Advertisement
The organ preservation or “watch and wait” approach is still a bit controversial, but a landmark study out of Brazil showed that the five-year cancer-specific survival was over 90%. A study from the Netherlands has reported on almost 1,000 patients treated with this approach with that number over 94%. Studies have shown the local tumor regrowth rate to be around 20 to 25%, and almost all of these were salvageable with curative-intent surgery with overall good oncological and perioperative outcomes. An important question is whether patients with a local regrowth following nonoperative treatment are at increased risk for metastases when compared with patients who undergo surgery immediately following neoadjuvant therapy. While we’re still awaiting results from several randomized trials, including the OPRA trial, this approach appears to offer significant advantages for patients.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5bb346eb-6e67-42e4-9394-3dfe34221110/20-DDI-1851913-expostedStomaIleostomy_650x450_jpg)
However, it is important that the “watch and wait” approach only be offered in the setting of an expert multidisciplinary team to ensure proper patient selection and meticulous long-term surveillance.
Dr. Liska: Right now, I am working with Matthew Kalady, MD, and others to understand the causes underlying the differences in treatment responses. We currently have no way to predict which patients will respond to TNT to select patients for this treatment course. Furthermore, there is currently no 100% reliable method apart from surgical resection to determine which patients have sustained a complete pathological response after neoadjuvant therapy.
Advertisement
On the molecular level, we are exploring are cancer-associated fibroblasts (CAFs). CAFs are a subpopulation of cells that reside within the tumor microenvironment and encourage tumor growth, angiogenesis, inflammation and metastasis. They also affect the response of colorectal cancer cells to cytotoxic drugs and targeted therapies. We have found that these cells also play an important role in the rectal cancer response to neoadjuvant therapy.
In addition, together with Cleveland Clinic colleagues Alok Khorana, MD, Smitha Krishnamurthi, MD, and Sudha Amarnath, MD, we will soon start enrolling in a VeloSano-funded clinical trial that will combine immunotherapy with chemoradiation to determine if we can personalize neoadjuvant therapy and achieve higher response rates.
Lastly, we are also collaborating with George Stark, PhD, on using a novel drug called CBL0137 to augment the effect of neoadjuvant therapy in rectal cancer.
Our goal is to use molecular markers to personalize multimodal treatment regimens that will maximize response rates, improve survival and allow for the safe selection of patients for organ preservation.
Advertisement
Advertisement

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists

Structured interventions enhance sleep, safety and caregiver resiliency in high-acuity units

Addressing rare disease and challenging treatment course in an active young patient