Newer technique is more efficient and good for patients
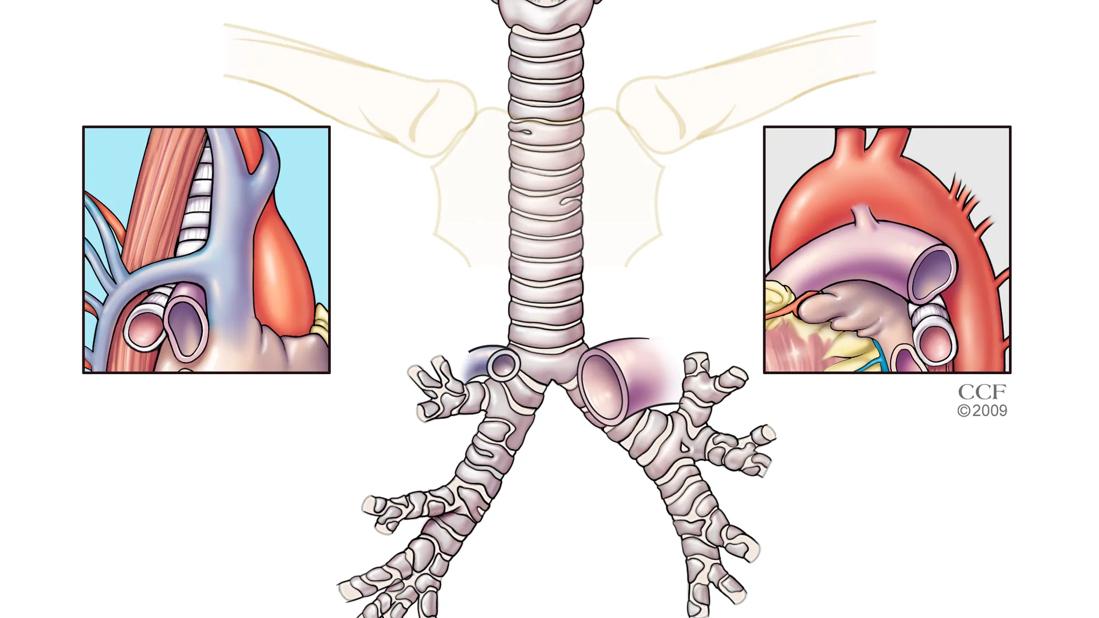
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/492b839d-f0b7-4bb9-84a5-bbd481693da3/Trachea-regional-anatomy-21513-jpg)
Trachea
Tracheotomy, that common surgical procedure performed to open a life-threatening airway obstruction or help critically ill patients wean from mechanical ventilation, traces back to ancient Egypt. In modern medicine, the basic procedure for the open surgical tracheotomy (OST) was introduced in 1909. Today’s medical realities, however, are driven by patient-centered care with a nod toward technology and more cost-effective care.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In the mid-1980s, as technology helped to improve outcomes in intensive care units (ICUs) and interest in minimally invasive procedures was growing, a new procedure that could be performed at the bedside was introduced—the percutaneous dilatational tracheotomy (PDT).
“The PDT has gained popularity because the patient can remain in the ICU setting,” explains Paul Bryson, MD, Director of the Cleveland Clinic Voice Center and Head of the Section of Laryngology at the Head & Neck Institute. “The increase in PDT procedures is driven by the ability to have the procedure done sooner, right there at the bedside—without waiting for an operating room (OR). It helps move patients to rehabilitation sooner, which is a good thing.”
Dr. Bryson and colleagues recently published a 6-year study on the shift from OST, which is performed in the OR under general anesthesia, to PDT, which is typically performed at the bedside in the ICU by trained intensivists, otolaryngologists, general and thoracic surgeons, interventional pulmonologists, and other non-surgical specialists. The study findings mirror those of other institutions that have seen tracheotomy procedures be shared by different specialties and also move from the OR to the ICU.
Results from the Cleveland Clinic study showed that tracheotomies performed by otolaryngologists declined by 3.4 percent per year from 2010 to 2015. While tracheotomies performed by thoracic surgeons (mostly on cardiothoracic patients already in the OR) stayed relatively steady, the number performed by general surgeons increased by 4.4 percent per year.
Advertisement
Furthermore, there was a dramatic increase in the number of PDT procedures by both the thoracic and general surgeons, with general surgeons performing an increasing number of bedside PDT procedures (Figure). Interestingly, no otolaryngologist performed a PDT during the 6-year study period at Cleveland Clinic. Within Otolaryngology, the decision to perform OST or PDT is based on surgeon preference.
According to the study, PDT has become more common due to a shortened procedure time, an ability to be done at the bedside, and a proven noninferiority safety profile, plus a potentially cheaper cost. However, Dr. Bryson notes that while initial complications from both surgeries are comparable, late complications from PDT—tracheal stenosis, tracheal fistulas and tracheomalacia—can be difficult to repair and may result in readmission, repeat tracheotomy, repeat airways dilations or surgeries, and possibly even open reconstructive surgery. Treating such complications falls to otolaryngologists due to their advanced understanding of head and neck anatomy.
“There will always be a need for otolaryngologists to perform OST, as it may be the only option for larger patients, the medically frail, or those with difficult anatomy,” he explains, noting the paper concludes with a call for improving patient safety by examining the follow-up and long-term care planning for trach patients. “Otolaryngology ultimately is the specialty that will be the final patient home for patients with complicated tracheotomies. But opportunities exist in all specialties and with all caregivers who care for patients with tracheotomies to improve safety and patient quality of life.”
Advertisement
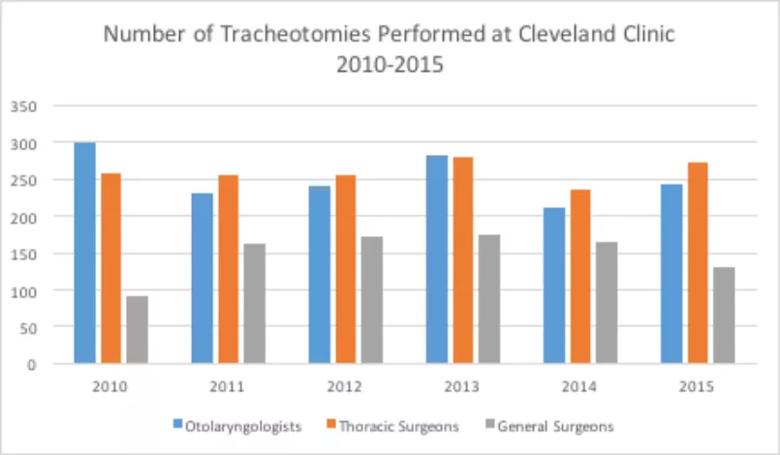
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/7df46934-fd76-48e2-b681-929b29f57f2f/18-ENT-670-Bryson-Inset-Graph-805pxl-width_jpg)
Bowen AJ, Nowacki AS, Benninger MS, Lamarre ED, Bryson PC. Is tracheotomy on the decline in otolaryngology? A single institutional analysis. Am J Otolaryngol. 2018;39(2):97-100.
Advertisement
Advertisement
Analysis of HNSCC patients shows HPV status to be predictive of higher abundance of oncobacteria within the tumor
Case study illustrates the potential of a dual-subspecialist approach
Evidence-based recommendations for balancing cancer control with quality of life
Study shows no negative impact for individuals with better contralateral ear performance
HNS device offers new solution for those struggling with CPAP
Patient with cerebral palsy undergoes life-saving tumor resection
Specialists are increasingly relying on otolaryngologists for evaluation and treatment of the complex condition
Detailed surgical process uncovers extensive middle ear damage causing severe pain and pressure.