The pulse of progress in percutaneous mitral, tricuspid and pulmonary valve procedures
As transcatheter aortic valve replacement (TAVR) has exploded in popularity since its 2011 FDA approval for commercial use (see related post here), it has drawn the lion’s share of attention around percutaneous heart valve care. But progress in transcatheter procedures for mitral, tricuspid and pulmonary valve disease has continued apace, even if a bit less prominently. To gauge that progress and learn what’s on the horizon, Consult QD asked several Cleveland Clinic experts to weigh in on developments to watch in the transcatheter space when it comes to the mitral, tricuspid and pulmonary valves. Highlights are below.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
1) Percutaneous approaches to degenerative disease. Degenerative mitral regurgitation (MR) is not a huge area of opportunity for transcatheter approaches since it’s already treated successfully with mitral valve repair surgery. Moreover, leading centers like Cleveland Clinic increasingly offer minimally invasive robot-assisted surgical repair. Still, a percutaneous approach holds appeal for some elderly patients and for individuals who want even less-invasive options.
That appeal has fueled development of two off-pump, transapical, echo-guided options for minimally invasive mitral valve repair through use of artificial chords. The two systems, known as NeoChord DS1000 and Harpoon, are intermediate steps toward percutaneous repair in that they involve a mini-thoracotomy, but both offer the potential for faster recovery than surgery. Both systems will be assessed in clinical trials that compare them to surgery, with Cleveland Clinic’s Cardiothoracic Surgery Chair A. Marc Gillinov, MD, involved in the Harpoon trial.
2) Percutaneous repair of functional MR. The big news in this space is the multicenter COAPT trial of the commercially available MitraClip® device. As reported in September (and recapped here), the study found that transcatheter mitral valve repair with MitraClip significantly reduced all-cause mortality and hospitalization compared with medical therapy in symptomatic patients with heart failure and secondary MR.
“COAPT has changed the paradigm,” says Cleveland Clinic’s Section Head of Interventional Cardiology, Samir Kapadia, MD, one of COAPT’s lead investigators and a member of its steering committee. “It’s the first large trial to show that treating functional MR not only makes patients feel better and prevents further worsening of the regurgitation, but also prevents death. This has fueled enthusiasm for treating functional MR with percutaneous repair, whether by targeting the annulus or leaflets.” A variety of investigational transcatheter approaches are being studied, including:
Advertisement
“The COAPT findings and all these similar investigational efforts are highly welcome, since functional MR is the area of mitral valve disease where treatment options have been most limited, including from a surgical perspective,” says Cleveland Clinic cardiac surgeon Stephanie Mick, MD.
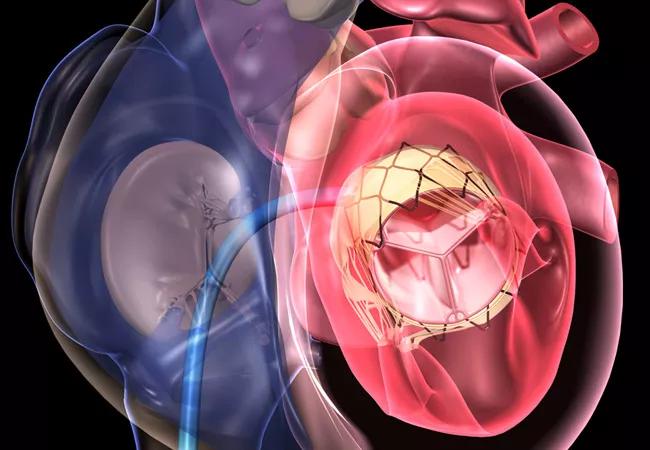
3) Percutaneous mitral valve replacement. Transcatheter valve replacement is also an option for mitral valve disease, but it’s more challenging than with aortic valve disease, as the native mitral valve can’t simply be pushed aside without risking left ventricular outflow tract obstruction. Anchoring of the valve in the correct position and delivery of devices also raise significant challenges. For these reasons, establishing safety and reproducibility will take longer for transcatheter replacement than for transcatheter repair in the mitral valve setting.
Nevertheless, several replacement technologies are in development for patients with degenerative or functional MR. These include the Cleveland Clinic-developed Navi™ mitral valved stent, which is not yet implanted entirely percutaneously but ultimately will be. Two options are delivered transapically — the Intrepid™ device, being studied in the multicenter APOLLO trial, and the Tendyne Mitral Valve Replacement System, being studied in the international SUMMIT trial, in which Cleveland Clinic is participating. Two additional options are delivered transseptally — the CardiAQ™ system and the Caisson system, both in feasibility studies involving or led by Cleveland Clinic.
Advertisement
“Key questions in the coming years include which patients are candidates for transcatheter mitral valve replacement and which for transcatheter mitral valve repair,” says Dr. Kapadia. “That’s a central issue to keep an eye on.”
4) Transcatheter valve-in-valve mitral valve replacement. Cleveland Clinic and a few other centers are successfully inserting replacement valve prostheses via catheter in patients with degeneration of a prior mitral valve prosthesis or ring. “We’re now doing valve-in-valve mitral valve replacements fairly regularly, with the patient under conscious sedation,” explains Dr. Kapadia. He expects this practice to spread — and with good reason. “Mitral valve reoperations are quite difficult and arduous for patients,” he says. “So this is an important advance.”
In the tricuspid valve arena, the key question to watch over the next few years is whether any single device can combine two essential criteria: (1) completely percutaneous implantation, and (2) complete elimination of tricuspid regurgitation (TR).
The current crop of devices and procedures succeed on one but not both fronts. Transcatheter tricuspid valve repair approaches — which involve either annular repair, clip-based leaflet repair, the Kay annuloplasty technique to improve coaptation, or placement of a spacer device — have shown success in improving patients’ quality of life and significantly reducing TR but not eliminating it.
Meanwhile, the leading transcathether tricuspid valve replacement approach — implantation of the GATE™ tricuspid valved stent — has successfully reduced TR to nonexistent or trivial levels in most of the 26 high-risk patients treated with it to date. Four of those patients — including the first in the world — were treated at Cleveland Clinic by a team led by cardiac surgeon Jose Navia, MD, and Dr. Kapadia, as detailed in this Consult QD post. The catch is that current delivery of the GATE valved stent is not completely percutaneous for a large number of patients, as it requires a transatrial approach and mini-thoracotomy in most patients. Notably, the first totally percutaneous tricuspid valve replacement in humans was performed by the same investigators at Cleveland Clinic.
Advertisement
“We’re working to reduce the size of the GATE delivery system so it can be fully percutaneous,” says Dr. Navia, who is the inventor of patents related to the device. Meanwhile, feasibility studies of this replacement system are likely to start in the U.S. and Europe in 2019.
Transcatheter pulmonary valve replacement (TPVR) is among the earliest percutaneous valve procedures, and it’s been established as a safe alternative to surgery in selected patients with congenital pulmonary valve and right ventricular outflow tract (RVOT) abnormalities.
In the setting of the native RVOT, such as in patients with tetralogy of Fallot after transannular patch repair, the dynamic RVOT — with its dilated, compliant and muscular nature — adds complexity to the TPVR procedure. Despite this, the established Melody and Sapien valves can be safely used in native RVOTs up to 29 mm in size. “The problem,” says Cleveland Clinic interventional cardiologist and adult congenital heart disease (CHD) specialist Joanna Ghobrial, MD, “is that many native RVOTs become considerably dilated beyond that dimension.”
Dr. Ghobrial notes that the newer valve systems currently in clinical trials — such as the Harmony valve, the Venus P valve and the Altera RVOT reducer — can accommodate dilated native RVOTs, which should substantially expand the realm of TPVR in CHD patients. “As these systems become commercially available, a much larger group of patients with CHD will benefit from the reduced invasiveness of transcatheter techniques for pulmonary valve replacement,” she says. “The result should be decreased morbidity and improved outcomes.”
Advertisement
Advertisement

Introducing Krishna Aragam, MD, head of new integrated clinical and research programs in cardiovascular genomics

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients

Multimodal evaluations reveal more anatomic details to inform treatment