Experienced team, innovative treatment
By Cristiano Quintini, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
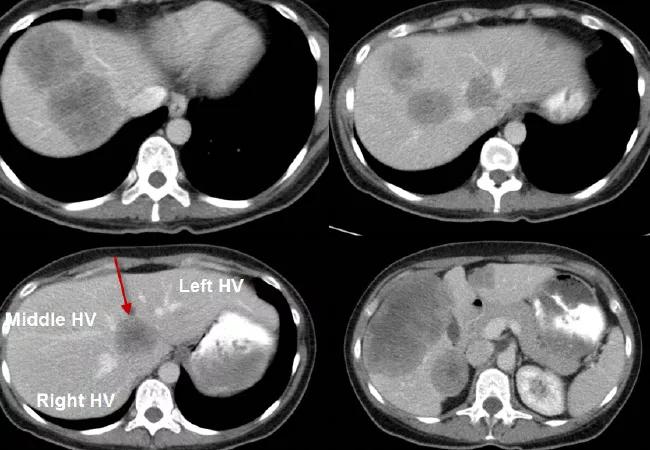
A 42-year-old female was referred to our institution with large right colon cancer and synchronous bilobar liver metastasis (see presenting CT scan of the liver above). A particular challenge was presented by the lesion encasing the three hepatic veins of the liver (see arrows).
The patient received three months of perioperative chemotherapy and was scheduled (three months after the initial presentation) for a two-stage hepatectomy and a combined resection of the primary right colon tumor.
The first surgery included a right hemicolectomy with resection of all the left-sided liver lesions. The surgery was uneventful. On postoperative day 6, the patient underwent a right portal vein embolization with the intent to induce hypotrophy of the right hemi liver and the hypertrophy of the left hemi liver. This approach is used to decrease the risks of postresection liver failure.
Six weeks after the first operation, the patient underwent a right hepatectomy. Given her young age and the extent of the disease, the decision was made to place to also place a hepatic artery infusion (HAI) pump to further decrease her likelihood of recurrence. HAI locoregional treatment is an innovative approach that improves survival after liver resection for metastatic colon cancer. This treatment option is only delivered in selected centers around the world.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/336ab2a6-d780-428c-bfa0-43a6027e8fe5/17-DDI-3877-Quintini-CQD-Inset1_jpg)
The remnant left liver lobe with a catheter inside the gastro-duodenal artery for HAI treatment.
One year after the initial presentation, the patient is free of tumor (see scan below) and receiving routine follow-up scans.
Advertisement

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/375db05f-5da2-45c9-9963-5600dbbcf5ee/17-DDI-3877-Quintini-CQD-Inset2_jpg)
CT scan showing the patient free of tumor.
Advertisement
Advertisement

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Potentially cost-effective addition to standard GERD management in post-transplant patients

Findings could help clinicians make more informed decisions about medication recommendations

Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care

Retrospective analysis looks at data from more than 5000 patients across 40 years

Surgical intervention linked to increased lifespan and reduced complications