Insights from 240 cases over 8 years at Cleveland Clinic
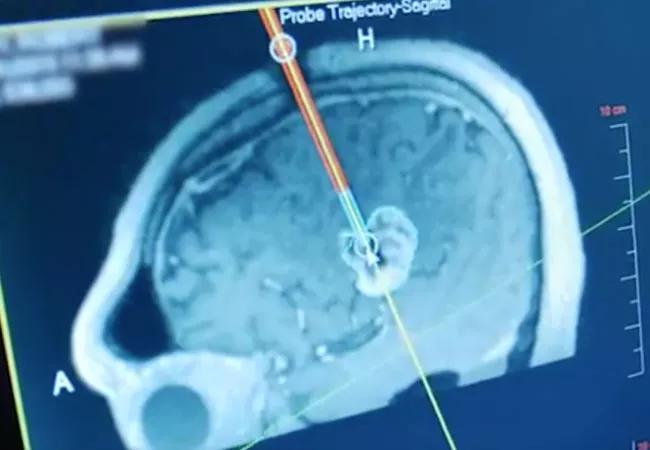
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a588036e-9069-4ad6-8de8-8a8aeb49a7c7/19-NEU-446-stereotactic-laser-ablation-brain-tumor-650x450_jpg)
19-NEU-446-stereotactic-laser-ablation-brain-tumor-650×450
Outcomes and operative times associated with stereotactic laser ablation for treating brain tumors dramatically improved over the past eight years at a single institution even as the procedure was increasingly used to treat metastases and radiation necrosis from radiosurgery failure. These findings — from a retrospective review of 240 Cleveland Clinic patients since 2011 — were detailed in a platform presentation this week at the 2019 annual scientific meeting of the American Association of Neurological Surgeons.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Cleveland Clinic was one of the early adopters of stereotactic laser ablation treatment for brain tumors, so we have good data starting in 2011, when the technology became commercially available after FDA approval,” says the study’s principal investigator, Alireza M. Mohammadi, MD, a neurosurgeon with Cleveland Clinic’s Rose Ella Burkhardt Brain Tumor and Neuro-Oncology Center. “Assessing our experience allows us to detect important trends and develop evidence-based best practices for other centers with more limited experience to follow.”
The study categorized patients into two time periods for comparison: the early period, from 2011 to 2014 (including 102 patients), and the more recent period, from 2015 to 2018 (138 patients). Extensive data on patient demographics, surgical and tumor characteristics, and temporary and permanent complications (the latter defined as unresolved after 6 months) were assessed.
The following differences were detected between the early and recent periods:
Advertisement
Dr. Mohammadi credits these substantial changes over the years to growing experience on the part of the multidisciplinary team as well as evolving technology. In 2013, a new generation of the state-of-the-art stereotactic laser ablation device (NeuroBlate® System) became available, allowing more efficient delivery of energy from the laser probe as well as improved planning and placement of the laser probe into the tumor.
Stereotactic laser ablation is a powerful tool that plays an increasing role in treating challenging brain tumors and their complications, Dr. Mohammadi notes. Some of the most important evolving applications include:
“We now have enough evidence to confidently say that stereotactic laser ablation can fill important roles for treating primary and metastatic brain tumors and radiation necrosis,” says Dr. Mohammadi. “We expect its uses to continue to evolve as technology advances, further enhancing our capabilities.”
Advertisement
Advertisement
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting
Radiation therapy helped shrink hand nodules and improve functionality
Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches