Formula works best for exophytic tumors
In an ideal world, urological surgeons would be able to predict how much kidney function patients would retain after partial nephrectomy (PN). This would improve patient counseling and could inform a variety of medical decisions, including whether to perform a radical nephrectomy (RN) or a PN.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Accurate prognostication, however, is difficult.
“When we perform a standard partial nephrectomy, a rim of normal parenchyma around the tumor is typically resected. During reconstruction, inevitably, some nephrons are devascularized and a certain amount of renal function will be lost,” says Steven Campbell, MD, PhD, Section of Urologic Oncology, Glickman Urologic & Kidney Institute. “The question is, ‘Can we predict how much function will be lost?’”
Other researchers have studied the contact surface area (CSA) between the tumor and the normal parenchyma, and have proposed that it correlates strongly with functional recovery after surgery. “When there is a greater surface area, more nephrons will be excised and the reconstruction will be more complex, so more parenchyma will be devascularized,” Dr. Campbell says.
Dr. Campbell and colleagues decided to conduct their own study with a larger cohort to explore the merits and limitations of CSA for predicting functional outcomes after PN (Figure 1).
“It is the largest, most comprehensive study in the literature to date,” he notes. Their findings were published in Urology and presented at the American Urological Association 2018 annual meeting.
Dr. Campbell and his co-authors analyzed medical records of 419 Cleveland Clinic pa-tients who underwent PN between 2007 and 2017. They measured parenchymal mass using contrast-enhanced computed tomography at less than two months prior and again at three to 12 months after PN. They calculated ipsilateral parenchymal mass preserved as final parenchymal mass normalized by preoperative parenchymal mass in the operated kidney.
Advertisement
Using the formula 2πrd, where r represents the tumor radius and d represents the in-traparenchymal depth of tumor, they estimated CSA. They also classified each case as either exophytic (≥ 50 percent extrarenal) or endophytic (> 50 percent intrarenal).
To estimate function, the team looked at serum creatinine levels and estimated global glomerular filtration rates (GFR). They examined global and ipsilateral function pre-served, defining them as final GFR normalized by preoperative GFR.
Timing: This study assessed functional parameters three-12 months after surgery to allow for complete healing and stabilization of the new baseline GFR. In other studies assessments were made much earlier, such as within the first month after surgery.
Substantial variance in tumor characteristics: This study had a median CSA value of 22.8 cm2, whereas in other studies median or mean CSA values were 14.5 cm2, 18.3 cm2 and 30.7 cm2.
More outcome parameters: This study looked at global and ipsilateral outcomes, both mass and function saved. The study also provided an analysis of the predictive utility of CSA in different cohorts of patients, namely those with endophytic versus peripherally located tumors.
Dr. Campbell’s team found that the association between CSA and GFR preserved by PN was much more modest than in previous studies. Correlation coefficients (r) be-tween CSA and functional outcomes were only in the range of 0.30-0.45, whereas moderate to strong correlations would be in the range of 0.5-0.8.
Advertisement
“Furthermore, we found that the formula worked fairly well to predict kidney function af-ter removal of exophytic tumors, but was less robust in predicting function after removal of endophytic tumors,” Dr. Campbell says.
“CSA is just too simple a metric to predict outcomes in complex cases involving resec-tion of endophytic renal tumors. Overall, our study suggests that CSA has substantial limitations and improved methods for predicting functional outcomes after PN are needed.”
Urology research fellow Chalairat Suk-Ouichai, MD, was co-author on this study.
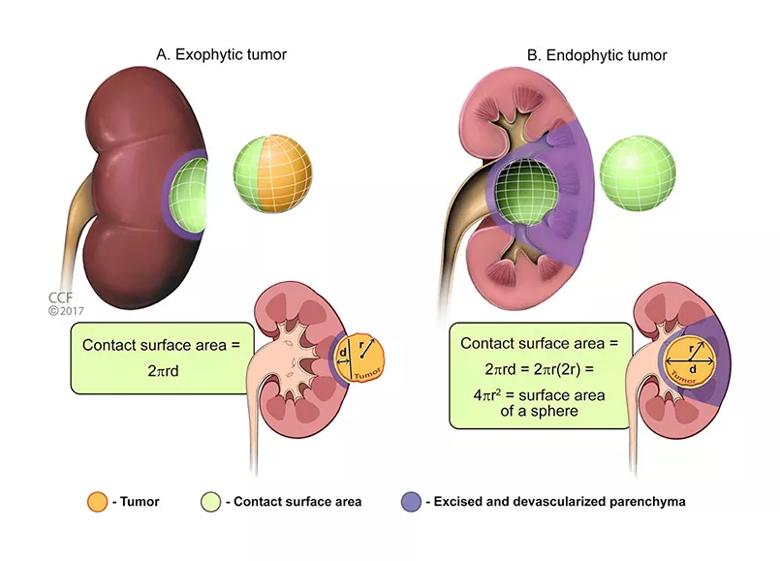
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/cb54cfd8-3145-4a7b-a487-fc5195ccae10/805x-Inset-exophytic-tumors_jpg)
Figure 1. Schematic of contact surface area (CSA, shown in green) between the tumor (orange) and normal parenchyma (red). Parenchymal mass that will likely be lost during standard partial nephrectomy (PN) is shown in purple. Loss of parenchymal mass consists of nephrons removed with the tumor and parenchyma that is devascularized during the reconstructive phase of the PN. For an exophytic tumor (A), the correlation between CSA and loss of parenchyma should be strong. For an endophytic tumor (B), additional parenchyma radial to the tumor will likely be devascularized or removed; therefore, CSA and loss of parenchyma may not correlate as strong-ly. Also, endophytic tumors are often closer to significant branch arteries, which could be inad-vertently compromised during renal reconstruction. If these arteries are supplying adjacent parenchyma outside of the purple zone, this would lead to further devascularization, again beyond what would be predicted by CSA. CSA can be estimated by the formula 2πrd, where r = radius and d = intraparenchymal depth of tumor, assuming that the tumor approximates a sphere, as previously described.
Advertisement
(Reprinted from Urology, pii:S0090-4295(18)30188-2. Chalairat Suk-Ouichai, Jitao Wu, Wen Dong, Hajime Tanaka, Yanbo Wang, J.J.H. Zhang, Elvis Caraballo, Erick Remer, Jianbo Li, Sudhir Isharwal, Steven C. Campbell; Tumor contact surface area as a predictor of functional out-comes after standard partial nephrectomy: utility and limitations; 6 March 2018. [Epub ahead of print], with permission from Elsevier.)
View Dr. Suk-Ouichai’s biography and those of our other residents and fellows.
Advertisement
Advertisement

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists