Multicenter study finds en bloc removal is preferable to piecemeal
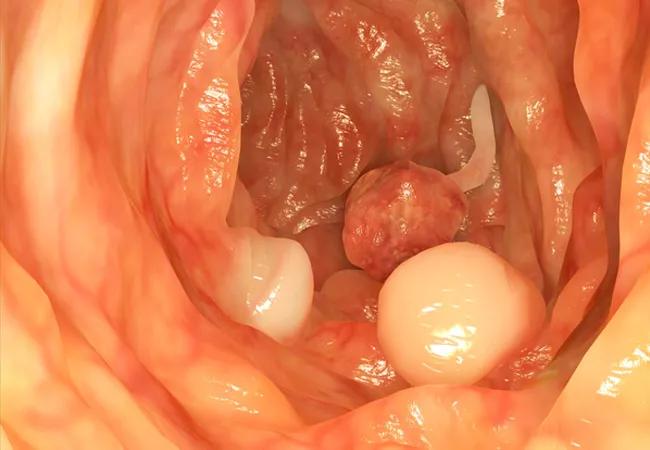
The etiology of a patient’s ampullary adenoma (AA) as well as the manner in which the lesion is resected are factors that affect the risk of recurrence, according to the largest retrospective multicenter study on the topic to date.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
AA recurrence rates after endoscopic papillectomy are higher in patients with after the first year of follow-up than in those with sporadic cases, the study involving Cleveland Clinic and 10 other institutions found. Piecemeal resection of the lesion also is associated with increased likelihood of recurrence.
Researchers from the Cleveland Clinic Digestive Disease & Surgery Institute’s Center for Advanced Endoscopy and the Sanford R. Weiss, MD, Center for Hereditary Colorectal Neoplasia presented the findings at the 2022 Digestive Disease Week annual meeting.
AAs are rare precancerous lesions. Patients with FAP-associated lesions face a heightened risk of ampullary carcinoma. Endoscopy is the primary means of therapeutic management for most AA cases. Few data exist about the comparative efficacy, safety and durability of minimally invasive endoscopic papillectomy for FAP-associated versus sporadic AA and the risk factors for post-procedure recurrence. The study’s goal was to assess variables in FAP and sporadic case cohorts.
“The majority of cases of ampullary adenoma we see at Cleveland Clinic are in patients who previously underwent resection, which raises the question as to how effective the technique is,” says gastroenterologist and study coauthor Amit Bhatt, MD. “To try to answer it, we needed to do a multicenter study. The results suggest that it is best to take the tumor out en bloc rather than to do piecemeal resection.”
To help fill the void in AA literature, the researchers conducted a study of 257 patients who underwent endoscopic papillectomy for the condition at 8 tertiary hospitals in the United States and one in India. One hundred patients (39%) had FAP; 157 patients (61%) had sporadic AA.
Advertisement
The researchers collected data retrospectively on demographics, type of AA, histologic characteristics, adverse events (AEs), time to first documented recurrence and last endoscopic follow-up. Follow-up data for three patients were not available.
The two types of resection evaluated were simple snare papillectomy or endoscopic mucosal resection, i.e. hot-snare papillectomy after submucosal fluid injection.
AEs were classified as intra-procedure, early post-procedure (≤14 days after endoscopic papillectomy) and late (>14 days after endoscopic papillectomy). Adenomatous tissue at the resection site within 4 weeks of papillectomy was considered residual tissue, not AA recurrence.
“By comparing outcomes of resection in patients with FAP-associated versus sporadic ampullary adenoma, we hypothesized that we could identify differences between the groups that would help dictate longer-term management,” says Dr. Bhatt. “What we found was an exceedingly high recurrence rate in both groups.”
At median follow-up of 22 months, 50 patients (26.5%) experienced recurrence of AA. The recurrence rate was 48% in patients with FAP compared with 37%% in those with sporadic disease. Patients with sporadic AA cases were more likely to have advanced histology and seven of them developed adenocarcinoma.
“The patients with sporadic ampullary adenomas actually had more advanced histology at the time of diagnosis compared to those with FAP,” says Cleveland Clinic gastroenterology fellow Achintya Singh, MD, the study’s first author. “That was an important finding because it indicates a difference between these tumors in terms of their aggressiveness.”
Advertisement
Regression analysis revealed that factors linked with risk of recurrence were FAP-associated AA after 12 months of follow-up (hazard ratio [HR] 2.2, 95% confidence interval [CI] 1.13-4.5) and bile duct dilation (HR: 20.4, 95% CI 1.2-3.4) while en bloc resection (HR 0.63, 95% CI 0.4-0.9) and use of endoscopic mucosal resection (HR 0.58, 95% CI 0.37-0.91) reduced the risk of recurrence.
“Recurrence of ampullary adenoma after endoscopic papillectomy was higher in FAP-associated than sporadic disease in spite of larger baseline size and more advanced histology of baseline ampullary adenoma in sporadic cases,” says Dr. Bhatt. In addition, use of simple snare papillectomy and piecemeal AA resection appeared to increase risk of recurrence.
According to Dr. Bhatt, the study’s results should underscore for clinicians the very risky nature of endoscopic papillectomy for ampullary adenoma and the potential for serious AEs associated with the procedure. He encourages them to “have honest conversations with their patients about the risk of recurrence and consider waiting and watching for a longer period of time before performing resection when the indication for endoscopic papillectomy is borderline.”
In patients who do undergo endoscopic papillectomy, en block resection is recommended and close follow-up for at least 1 year post-procedure is warranted.
“I think the study would support, whenever possible, use of endoscopic mucosal resection for ampullary adenomas, and preferably tumor removal en bloc,” Dr. Singh says.
Advertisement
In terms of future research on ampullary adenoma, areas of investigation for the Cleveland Clinic team include the efficacy of specific treatments and new technologies such as radiofrequency ablation and initiatives aimed at better understanding the natural history of the disease.
Advertisement
Advertisement

Benefits of neoadjuvant immunotherapy reflect emerging standard of care

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Potentially cost-effective addition to standard GERD management in post-transplant patients

Findings could help clinicians make more informed decisions about medication recommendations

Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care

Retrospective analysis looks at data from more than 5000 patients across 40 years