Research needed to fill critical knowledge gaps
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
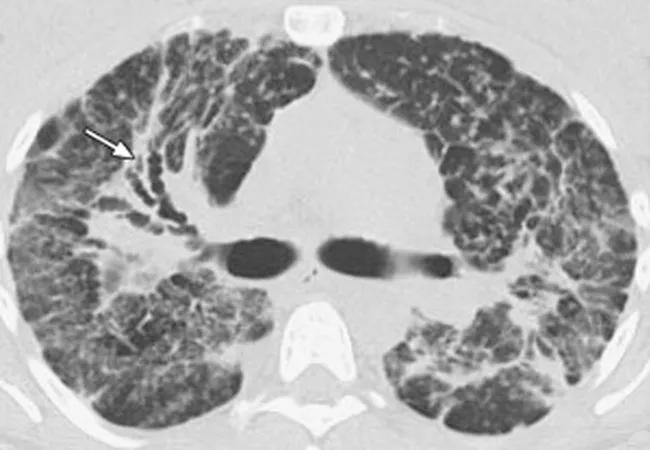
Treatment-resistant pulmonary disease — primarily pulmonary fibrosis and pulmonary hypertension — contributes to pulmonary disease being the most common cause of death in sarcoidosis. Radiologically overt pulmonary fibrosis develops in five to 10 percent of patients with sarcoidosis. Pulmonary hypertension develops in the same percentage; however, the complication is found in more than 50 percent of sarcoid patients with persistent dyspnea.
Although the majority of patients with limited pulmonary fibrosis never develop severe disease, we have no validated markers to help predict which patients will progress to significant fibrosis, and the value of imaging findings in predicting treatment or outcome is unknown. Additionally, how treatment for pulmonary sarcoidosis might mitigate risk is unknown.
A model that combines physiological and radiographic parameters to better predict mortality in these patients has been developed, but requires validation in a large population. While the signs and symptoms suggestive of pulmonary hypertension have been identified, they also require further validation, since many of the individual risk factors are also associated with other lung diseases.
In late 2015, I participated in a National Heart, Lung, and Blood Institute sarcoidosis workshop as part of a multidisciplinary team that reviewed known data on patients with manifestations of high-risk sarcoidosis and suggested where research efforts should be targeted. Our conclusions led us to make the following recommendations in a 2017 article in Annals of the American Thoracic Society:
Advertisement
Cleveland Clinic’s Sarcoidosis Clinic is a World Association of Sarcoidosis and Other Granulomatous Disorders (WASOG) member. In this capacity, we provide multidisciplinary care to patients with all forms of sarcoidosis, while developing new treatment approaches through research.
We encourage you to refer patients with a high suspicion of, or diagnosed with, pulmonary sarcoidosis for a second opinion. Evaluation by our experienced multispecialty team often reveals overlooked aspects of the disease that require attention. We are able to offer a variety of treatments beyond steroids, as well as participation in clinical trials. These are key aspects of care that minimize the degree to which treatment-resistant pulmonary fibrosis affects quality of life.
Dr. Culver directs both the Interstitial Lung Disease and Sarcoidosis Programs the in the Department of Pulmonary Medicine at Cleveland Clinic.
Advertisement
Advertisement

Takeaways from the most recent annual meeting centered around clinical advances, AI integration and professional development

Recent breakthroughs have brought attention to a previously overlooked condition

A review of treatment options for patients who may not qualify for surgery

Looking at the real-world impact and the future pipeline of targeted therapies

The progressive training program aims to help clinicians improve patient care

New breakthroughs are shaping the future of COPD management and offering hope for challenging cases

Exploring the impact of chronic cough from daily life to innovative medical solutions

How Cleveland Clinic transformed a single ultrasound machine into a cutting-edge, hospital-wide POCUS program