Which cysts turn malignant and why NSAIDs can be chemoprotective
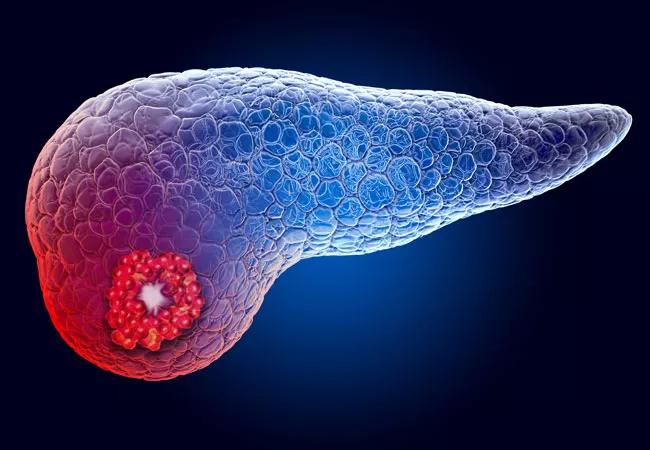
Pancreatic cancer is the fourth leading cause of cancer death in the United States. With no surveillance method for early detection, patients often present at an advanced stage, when surgery is no longer an option.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Certain benign pancreatic cysts carry malignant potential of varying degrees. Recommendations for the diagnosis and surveillance of these cysts, and when to refer patients for surgery, are based on low-quality evidence. Data on the underlying risk factors for these cysts and predictors of growth, malignancy and need for surgery are also limited.
Cleveland Clinic gastroenterologists sought to add to this body of knowledge by studying the natural history of pancreatic cysts and identifying predictors of increased growth and high-risk transformation.
We spoke with gastroenterology fellow Mohannad Abou Saleh, MD, and principal investigator Prabhleen Chahal, MD, Program Director of Advanced Endoscopy Fellowship, about the study and its implications for patient care.
How did you go about studying pancreatic cysts?
Dr. Abou Saleh: We established a registry of all patients with pancreatic cysts seen on imaging at Cleveland Clinic starting in 2008. With more than 1,000 entries, it is one of the largest pancreatic cyst databases in the country.
Do we know which cysts become malignant?
Dr. Abou Saleh: Pancreatic pseudocysts do not become malignant. Malignant cysts include solid-pseudopapillary neoplasm and cystic pancreatic neuroendocrine tumor. Benign cysts with malignant potential include intraductal papillary mucinous neoplasms (IPMN) and mucinous cystic neoplasms. Among IPMN, main-duct IPMN and mixed-type of IPMN carry an increased risk of malignant transformation, with reports of up to 62% (range 36-100%) in patients undergoing surgical resection. The risk is much lower in branch-duct IPMN, with a lifetime malignancy risk of around 2.8%.
Advertisement
When is surgery indicated?
Dr. Abou Saleh: That is an important question and one of the reasons why we established a database, as there is no consensus. This is why the decision for surgery is usually made after careful evaluation by a multidisciplinary team.
We evaluate patients with abdominal imaging and, in some patients, endoscopic ultrasound to look for high-risk stigmata, such as a solid component within the cyst, pancreatic duct dilation or cyst size of 3 cm or greater. We obtain a fluid sample from the cyst and analyze it for tumor markers and cancerous or precancerous cells. If such cells are found, surgery is indicated.
We also review the patient’s symptoms. If the patient has jaundice or recurrent pancreatitis attributable to the cyst, surgery is indicated.
Apart from establishing an indication for surgery, it is important to determine whether the patient is fit for surgery. If the patient is not a surgical candidate, imaging surveillance may not be indicated.
How do you follow patients after surgery?
Dr. Abou Saleh: What should be done after surgery is not clear, as there are limited long-term studies on how these patients do and whether they have recurrences. Usually they have follow-up with abdominal imaging.
Your study found low body-mass index (BMI) correlates with increased risk for malignant changes in pancreatic cysts over time. Can you please elaborate on this?
Dr. Abou Saleh: This was a unique finding of our study, and the underlying pathophysiology of this association is uncertain. However, unintentional weight loss is often associated with malignancy, due to the catabolic state that cancer patients are in. This may explain our finding.
Advertisement
You also found a significantly decreased risk of growth in pancreatic cysts among NSAID users. Can you explain this?
Dr. Abou Saleh: Several studies looking at the chemopreventive role of NSAIDs in different cancers have suggested that NSAIDs can restore normal apoptosis and reduce cell proliferation, which is key in preventing cancer growth. Our study is the first to show the effect of NSAIDs on pancreatic cysts.
Dr. Chahal: Our finding of decreased risk of growth among premalignant cysts in patients on NSAIDs is promising. However, more long-term data are warranted to corroborate this finding.
If there’s no consensus regarding screening, surveillance or surgical intervention of pancreatic cysts, do you want to make a recommendation based on your study?
Dr. Abou Saleh: I think our study adds to the existing body of literature, and we are working on several extensions of the study to contribute further. Certainly, unintentional weight loss should prompt further investigation.
What is the key takeaway message? How can the results of your research help physicians improve patient care?
Dr. Chahal: Even though pancreatic cysts are often detected incidentally on imaging, it is important to take them seriously, because some carry malignant potential. An exhaustive process goes into carefully evaluating the nature of these pancreatic cysts, and timely referral and close follow up with a gastroenterologist is often warranted.
Advertisement
Advertisement

Benefits of neoadjuvant immunotherapy reflect emerging standard of care

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Potentially cost-effective addition to standard GERD management in post-transplant patients

Findings could help clinicians make more informed decisions about medication recommendations

Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care

Retrospective analysis looks at data from more than 5000 patients across 40 years