How to diagnose and manage care for patients affected by this condition

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/99e1a694-d531-4163-b26b-9f8ff8a36709/650x450-Dyspnea-2_jpg)
650×450-Dyspnea-2
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Dyspnea is a common complaint faced by primary care physicians, cardiologists and pulmonologists in the outpatient clinic. After a comprehensive diagnostic evaluation, the cause of dyspnea may remain elusive in 10%-20% of patients. A chronically low preload state may be responsible for the dyspnea in several of these patients. In chronically low preload states, there is insufficient venous return, which results in inadequate cardiac output and the development of symptoms such as dyspnea, particularly when standing or during exercise. The exact mechanism of dyspnea remains obscure, but plausible explanations include ventilation/ perfusion mismatch, respiratory muscle fatigue, skeletal muscle dysfunction, deconditioning and imbalance between respiratory neural drives and afferent feedback of the respiratory system.
Conditions associated with chronically low preload states can be broadly divided into three groups, including a decrease in intravascular volume, venous obstruction/restriction and reduction in venous tone. Increased venous capacitance and excessive blood pooling in the lower extremities are seen in patients with postural orthostatic tachycardia syndrome (POTS), orthostatic hypotension and small fiber neuropathy. The diagnosis of chronically low preload states as the reason for dyspnea involves a focused clinical history, including an evaluation of the autonomic system, determination of orthostatic vital signs, and tests to assess the cardiovascular, neurological and autonomic functions. Importantly, the mainstay of diagnosis requires invasive cardiopulmonary exercise testing (iCPET) (Figure).
Advertisement
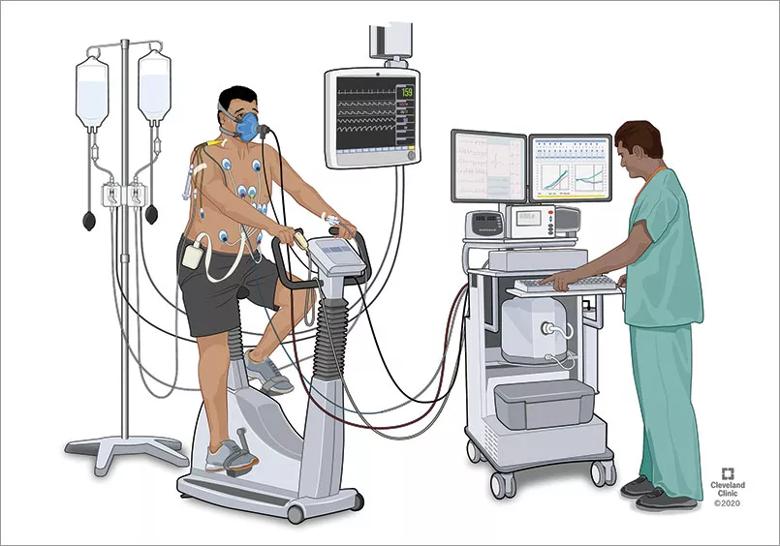
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/cf485ea0-c204-4e65-bbdb-2f77d9a87882/805x-Inset-Patient-Difficulty-Breathing-1_jpg)
Figure. Invasive cardiopulmonary exercise is the gold standard test for diagnosing chronically low preload states as the reason for dyspnea. Additionally, a focused clinical history, including an evaluation of the autonomic system, determination of orthostatic vital signs, and tests to assess the cardiovascular, neurological and autonomic functions, should be obtained.
Preload is defined as the force to stretch fibers at the end-of-diastole and depends on several factors, such as ventricular dimension and compliance, wall thickness, transmural diastolic pressure, ventricular interdependence and venous return. When standing, there is a shift of 700 mL-900 mL of blood volume to the lower body that is counterbalanced by a reduction in venous compliance in combination with functional venous valves, muscle contraction and the suctioning action of the respiratory pump. The measurement of preload in vivo is challenging but can be estimated by the right atrial and pulmonary artery wedge pressure obtained during right heart catheterization (RHC).
The iCPET collects the traditional information provided by the CPET but adds simultaneous hemodynamic and gasometric information from pulmonary and radial artery catheterization. Therefore, the iCPET provides a comprehensive evaluation of ventilation, gas exchange and cardiac function at rest and during incremental exercise. There is no consensus regarding the hemodynamic definition of preload insufficiency, but the condition needs to be considered in cases of an unexplained abnormal cardiac limitation to exercise (peak oxygen consumption of < 80% of predicted and peak cardiac output of < 80% of predicted), combined with reduced ventricular preload (peak right atrial pressure < 9 mmHg, peak pulmonary artery wedge pressure < 14 mmHg, and peak pulmonary artery pressure < 30 mmHg).
Advertisement
The management of chronically low preload states requires a multidisciplinary team, including pulmonologists, cardiologists, neurologists, rheumatologists, exercise physiologists, and other professionals. The goal is to diagnose the condition, identify the cause of the chronically low preload state and provide the best treatment. Treatment requires a holistic approach, including nonpharmacological and pharmacological interventions. We aim to optimize the volume status by increasing hydration, salt intake and using over-the-knee or, ideally, waist-high compression stockings. Another critical component is exercise training with endurance and resistance training focused on the core and lower body. When nonpharmacologic measures are insufficient, we use medications, such as salt tablets and fludrocortisone, to increase blood volume, midodrine to increase sympathetic activity, pyridostigmine to increase peripheral cholinesterase, and other interventions. In certain inflammatory/autoimmune conditions, we consider intravenous immunoglobulin, rituximab, or other agents. In summary, dyspnea due to chronically low preload states should be considered in patients with unexplained dyspnea. The specific cause needs to be investigated by a multidisciplinary team to deliver the best treatment strategy.
Dr. Tonelli is staff in the departments of Pulmonary Medicine, Critical Care Medicine and Pathobiology.
Tooba R, Mayuga KA, Wilson R, Tonelli AR. Dyspnea in chronic low ventricular preload states. Ann Am Thorac Soc. Published online. December 2, 2020. doi: 10.1513/AnnalsATS.202005-581CME
Advertisement
Advertisement
Takeaways from the most recent annual meeting centered around clinical advances, AI integration and professional development
Recent breakthroughs have brought attention to a previously overlooked condition
A review of treatment options for patients who may not qualify for surgery
Looking at the real-world impact and the future pipeline of targeted therapies
The progressive training program aims to help clinicians improve patient care
New breakthroughs are shaping the future of COPD management and offering hope for challenging cases
Exploring the impact of chronic cough from daily life to innovative medical solutions
How Cleveland Clinic transformed a single ultrasound machine into a cutting-edge, hospital-wide POCUS program