When procedure is performed by high-volume surgeons, outcomes are comparable to total knee replacement

By Alvaro Ibaseta, MD, and Trevor G. Murray, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Prevalence of knee osteoarthritis is high and rising among U.S. adults, with demand for knee arthroplasty estimated to increase 600% by 2030.1 According to one study, 85% of cases present with isolated single-compartment degeneration, most commonly in the medial compartment.2
An alternative to total knee arthroplasty (TKA), unicompartmental knee arthroplasty (UKA) can preserve some ligaments and bone in patients with isolated single-compartment end-stage osteoarthritis. However, while an estimated 45%-50% of patients with knee osteoarthritis could be candidates for UKA, it is pursued in only 5%-8% of cases.2
Low adoption of UKA is attributed primarily to the long learning curve for surgeons as well as registry data that show high revision rates of UKA compared to TKA.3,4 However, recent data challenge conventional concerns and show that UKA is a safe and effective procedure that may be a better option for many patients.
UKA is less invasive than TKA and spares noninvolved ligaments and bone. The approach requires limited exposure and no dislocation of the knee joint, which results in significantly less soft-tissue damage (Figure 1). Operative time is shorter, blood loss is reduced, and hospital stays are decreased compared to TKA.
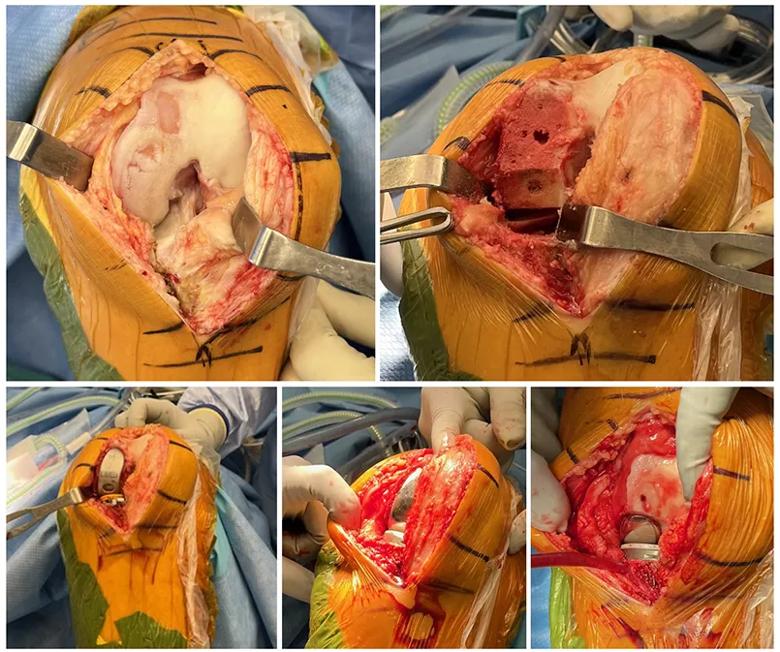
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/69d66996-4d3a-4050-bf30-b8e10a6b1314/22-ORI-3183858-CQD-inset1_jpg)
Figure 1. Intraoperative evaluation of isolated medial-compartment osteoarthritis and example of UKA’s ligament- and bone-sparing approach. The medial compartment is exposed and resurfaced, while the patellofemoral and lateral compartments are spared. The ACL and lateral meniscus remain intact, the patellar ligament is minimally disturbed, and the knee is never dislocated.
In the immediate postoperative period, patients achieve greater range of motion and a higher overall level of activity. In the longer term, UKA offers significantly higher rates of forgettable joints due to preservation of knee kinematics, preservation of bone stock and overall lower morbidity.2
Advertisement
Patient selection is considered crucial for long-term success of UKA. Conventionally, indications for UKA have been narrow, with the ideal patient being younger than age 60 and weighing less than 180 lbs., with isolated medial, lateral or patellofemoral osteoarthritis or osteonecrosis; correctable angular deformity less than 15 degrees; flexion contracture less than 5 degrees; and range of motion greater than 90 degrees. Patients have been considered nonideal if they have a high level of activity, exposed bone in the patellofemoral compartment, anterior knee pain, chondrocalcinosis, osteophytes in the opposite compartment, inflammatory arthritis or ACL insufficiency.
However, these conservative criteria are poorly backed by evidence. Multiple recent studies report successful results in patients formerly considered suboptimal for UKA.5
Overall, UKA has become a valid option for the younger patient as an alternative to high tibial osteotomy, showing lower rates of complication and reoperation. UKA is also a valid option for older patients, who may not recover as readily from a more invasive TKA. UKA offers reduced operative time, blood loss and hospital stays, and enables higher levels of activity at discharge.
As previously noted, early registry data showed high revision rates in UKA compared to TKA — a statistic that is frequently quoted when deciding against UKA. However, these data need careful interpretation. More recent cohort studies from high-volume centers report survivability of the modern UKA as similar to TKA.6
Advertisement
There are a number of factors that may explain this difference:
For the appropriately indicated patient, UKA can be a more effective and less invasive surgical option than TKA. Modern implants and surgical techniques in the hands of high-volume surgeons result in outcomes comparable or superior to TKA.
Medial UKA (Figure 2) is the most commonly performed and best understood UKA procedure, but any compartment can be replaced. At Cleveland Clinic, we have performed single-stage bilateral patellofemoral UKA (Figure 3).

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b8d697ab-ee3b-4c9e-9d68-847a3f1fdc35/22-ORI-3183858-CQD-inset2-975x1024_jpg)
Figure 2. Radiographic evaluation of isolated medial-compartment osteoarthritis successfully treated with medial UKA.
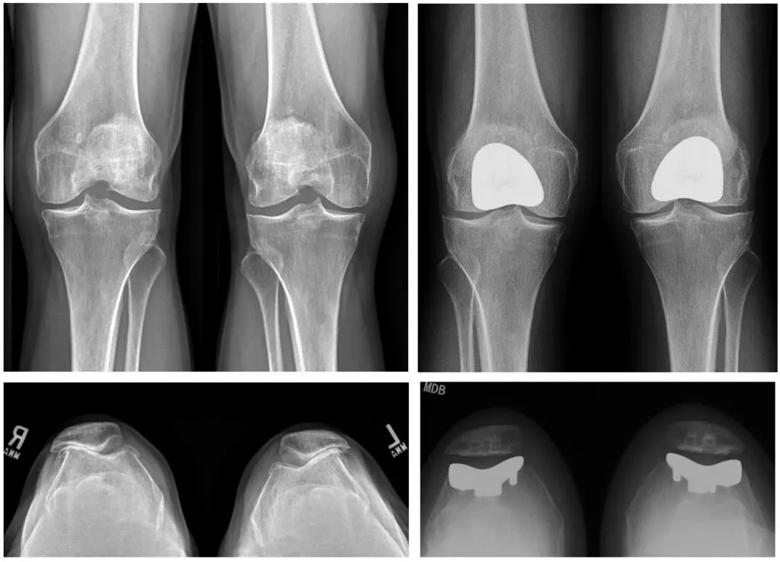
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/441360e5-7a3f-48a4-9be6-759e99d5c3ec/22-ORI-3183858-CQD-inset3-1024x738_jpg)
Figure 3. Radiographic evaluation of bilateral isolated patellofemoral osteoarthritis successfully treated with patellofemoral UKA.
Overall, we have been able to report excellent short- and long-term outcomes, almost-universal same-day discharge, quick surgical recovery, a high level of activity at discharge, and a low rate of complications. While there is a risk of eventual conversion to TKA, our data agree with the latest cohort results, showing similar survivability between UKA and TKA.
Advertisement
Dr. Murray is staff in the Department of Orthopaedic Surgery and a high-volume unicompartmental knee arthroplasty surgeon. Dr. Ibaseta is a resident in the Department of Orthopaedic Surgery.
References
Advertisement
Advertisement

Self-care may be just as effective for some patients

Most return to the same sport at the same level of intensity

More report a clinically meaningful change in function at 90 days compared to patients with lower BMI

How to diagnose and treat crystalline arthropathy after knee replacement

Special glasses allowed surgeon to see 3D models and anatomic data superimposed on surgical field

Study findings warrant caution in patients at risk for DVT, cardiovascular issues and more

Robot assistance turns two-stage surgery into a single procedure

Robot scores better in length of stay and home discharge; manual scores better in flexion and operative time