Cleveland Clinic geriatrician weighs in on new AA recommendations
In July, the Alzheimer’s Association (AA) released the first Clinical Practice Guidelines (CPG) for the evaluation of AD and other dementias. Saket Saxena, MD, geriatrician at Cleveland Clinic’s Center for Geriatric Medicine attended the AA annual international conference in Chicago in July where the clinical guidelines were presented.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
This AA workgroup developed 20 guidelines, ranging from recognizing and more effectively evaluating symptoms to compassionately communicating with and supporting affected individuals and their caregivers. The CPGs state that all middle-aged or older individuals who self-report, or whose care partner or clinician reports cognitive, behavioral or functional changes, should undergo a timely evaluation. Concerns should not be dismissed as a normal effect of the aging process.
Dr. Saxena says Cleveland Clinic has been following the regulations and guidelines of the Affordable Care Act since 2010, and that the new CPGs are “consistent with and simply reinforce” these earlier protocols.
“It is the new research framework that has been proposed that is most exciting,” Dr. Saxena believes. This new framework was jointly proposed by the National Institute of Aging (NIA) and the AA. The proposed framework by NIA-AA includes a goal of identifying dementia early by using dementia biomarkers-AT(N) biomarker grouping as follows:
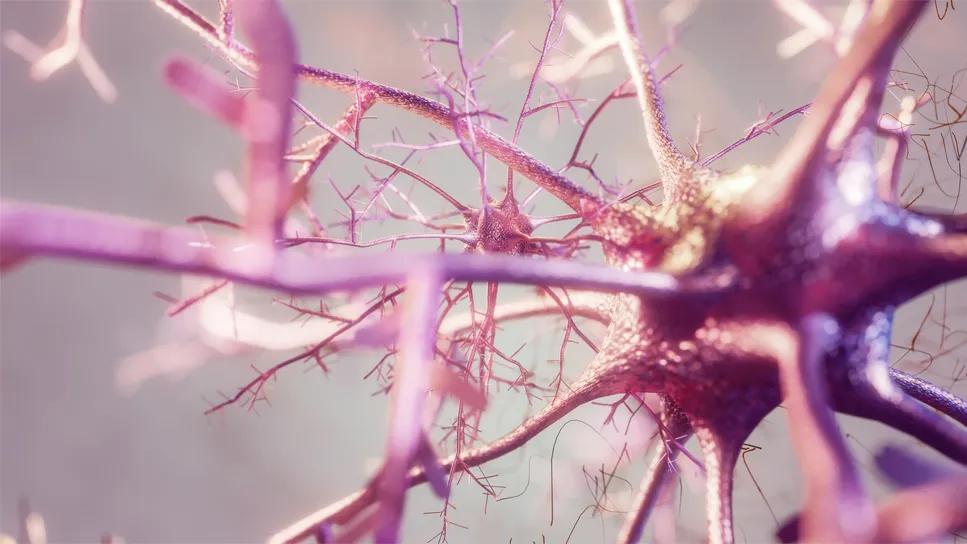
The biological construct proposed is “based on measurable changes in the brain and is expected to facilitate better understanding of the disease process and the sequence of events that lead to cognitive impairment and dementia,” according to the NIA. The framework will apply to clinical trials, as well as observational and natural history studies.
Advertisement
“Moving forward, research will focus heavily on neuropathic biomarkers of Alzheimer’s, which over time will bring more objectivity to our clinical suspicions and lead to potential treatments,” says Dr. Saxena. “How we incorporate the new thinking and tools into our research and ultimately in our clinical practice will be something new for the medical community, and it is definitely a step in the right direction.”
Tools include using advanced 3T MRI, cerebrospinal fluid (CSF) analysis, and PET imaging to improve diagnostic accuracy when warranted. And Dr. Saxena notes, “The use of newer diagnostic tests will increase as available research becomes more robust.”
Advertisement
Advertisement

Researchers explore the mental and physical benefits of social prescribing

Multidisciplinary approach helps address clinical and psychosocial challenges in geriatric care

Effective screening, advanced treatments can help preserve quality of life

Study suggests inconsistencies in the emergency department evaluation of geriatric patients

Auditory hallucinations lead to unusual diagnosis

How providers can help prevent and address this under-reported form of abuse

How providers can help older adults protect their assets and personal agency

Recognizing the subtle but destructive signs of psychological abuse in geriatric patients