When conventional ventilatory therapies aren’t enough
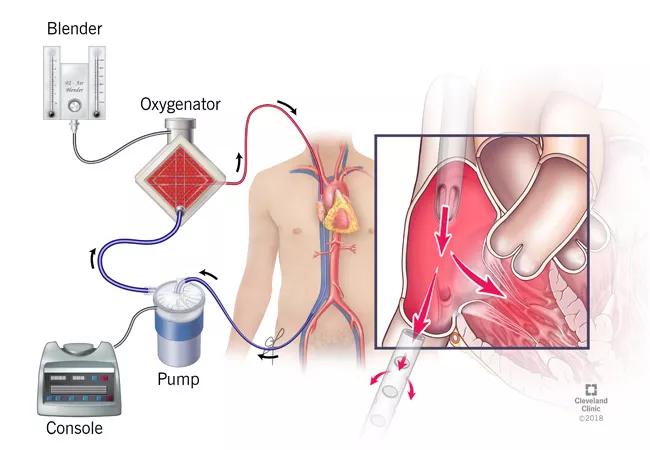
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d9b1488e-4aa4-4789-9790-88af400db53d/18-PUL-443-Krishnan-Hero-Image-650x450pxl_jpg)
18-PUL-443-Krishnan-Hero Image-650x450pxl
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Venovenous (VV) extracorporeal membrane oxygenation (ECMO) is a temporary mechanical assistance device that allows for prolonged cardiopulmonary support. A modification of the cardiopulmonary bypass machine, it is instituted in patients with life-threatening respiratory failure (predicted mortality 80 percent). ECMO is considered for patients with potentially reversible forms of respiratory failure and as a bridge to lung transplantation for suitable candidates with irreversible disease. The respiratory ECMO service at Cleveland Clinic was recently established as a 24/7 on-call service that facilitates the use of VV ECMO to manage ventilatory failure (refractory hypoxemia or hypercarbia) that is not amenable to conventional ventilatory support and adjunctive therapy (e.g., neuromuscular paralysis and prone ventilation).
The VV ECMO circuit (in its rudimentary form) consists of specialized cannulae attached to a conduit tubing connected to a centrifugal pump. Venous blood is siphoned into an extracorporeal artificial membrane oxygenator, and oxygenated blood is returned to the systemic venous circulation.
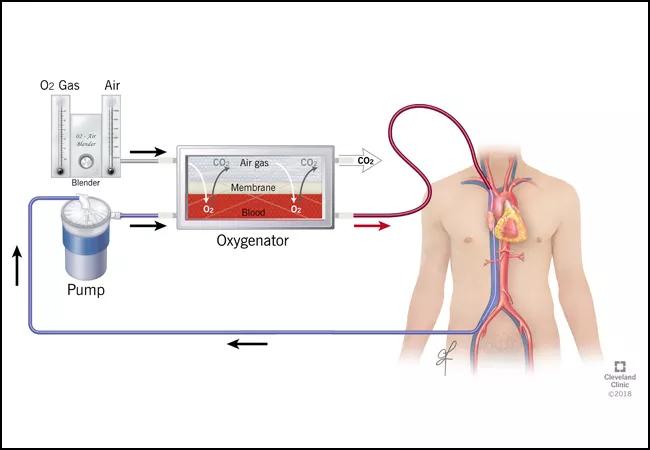
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a2571449-ff86-4762-ba62-6124f4b33502/18-PUL-443-Krishnan-Figure-01-650x450pxl_jpg)
The oxygenator consists of numerous low-resistance, hollow, nonmicroporous fibers that allow for oxygen transfer across a semipermeable membrane from gas to blood interphase. VV ECMO improves systemic oxygenation and provides for a reduction in ventilatory inflation pressures, thereby decreasing ventilator-induced lung injury and facilitation of lung recovery.
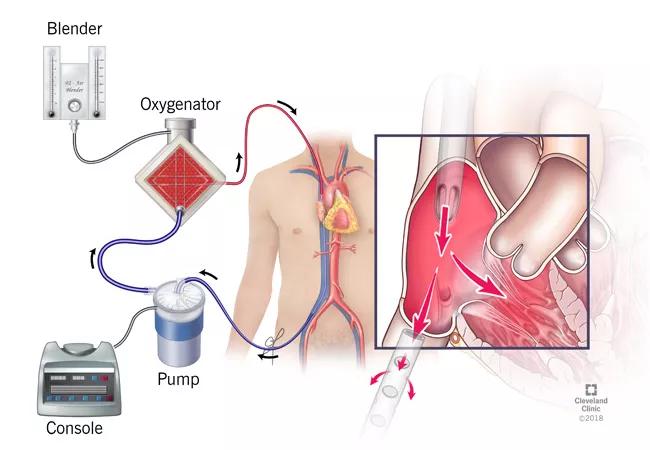
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/f459942a-3774-4400-b69d-e9e054c930fb/18-PUL-443-Krishnan-Figure-02-650x450pxl_jpg)
VV ECMO does not support systemic circulation or alter hemodynamics, in contrast to venoarterial ECMO.
Advertisement
ECMO is a resource-intensive endeavor associated with a high mortality rate (approximately 50 percent). In order to maximize the utility of this modality, its application should be restricted to those patients with a reasonable likelihood of survival either with supportive care (bridge to recovery) or lung transplantation (bridge to transplant).
Initiation of ECMO as a desperation measure should be avoided when factors suggesting futility are present. However, identifying patients with a reversible underlying condition is often a contentious and challenging task.
A selection process that identifies patients with an overall favorable prognosis who are likely to return to a highly independent functional status is integral to Cleveland Clinic’s respiratory ECMO program.
Appropriate timing, stringent selection criteria, and the use of clinical prediction models to estimate the likelihood of survival are integral to the process. Decisions about initiation of ECMO are made within the framework of active communication between the MICU team, medical and surgical ECMO staff, and the patient’s surrogate decision-makers.
Our medical ECMO team is staffed by members of our pulmonary and critical care departments with expertise in a wide range of pulmonary disorders, management of respiratory failure and lung transplantation. Bedside rounds are conducted in conjunction with members of the surgical ECMO team and anesthesia critical care team as well as respiratory therapists, perfusionists and pharmacists.
Advertisement
This multidisciplinary medical/surgical ECMO team is involved in decisions about initiation of ECMO, management of the patient while on the device and decisions to decannulate and transition to conventional ventilatory support or palliative care.
Recognizing that ECMO survivors face a long and often arduous road to full recovery, staff from our Department of Critical Care Medicine have initiated a post-ECMO care program for these patients. This involves a team that follows these patients after transfer out of the ICU until hospital discharge and the establishment of a post-ICU outpatient clinic to transition their care to the ambulatory setting and to address residual pulmonary, neuromuscular, cognitive and psychological dysfunction.
While awaiting the outcome of large clinical trials aimed at defining the group of patients most likely to benefit from ECMO, we will continue our judicious application of the modality to critically ill patients who are failing conventional support measures and whose disease is either deemed potentially reversible or amenable to transplant.
With our extensive experience with ECMO at Cleveland Clinic, we are poised to expand the role of this intervention as warranted by demonstration of efficacy. We believe that our dedicated ECMO team, multidisciplinary approach and commitment to provide longitudinal inpatient and outpatient care maximize the chances of successful outcome, minimize practice variation and avoid the indiscriminate use of this evolving technology.
Advertisement
Dr. Krishnan is staff in Critical Care Medicine and Pulmonary Medicine at Cleveland Clinic.
Advertisement
Advertisement
Takeaways from the most recent annual meeting centered around clinical advances, AI integration and professional development
Recent breakthroughs have brought attention to a previously overlooked condition
A review of treatment options for patients who may not qualify for surgery
Looking at the real-world impact and the future pipeline of targeted therapies
The progressive training program aims to help clinicians improve patient care
New breakthroughs are shaping the future of COPD management and offering hope for challenging cases
Exploring the impact of chronic cough from daily life to innovative medical solutions
How Cleveland Clinic transformed a single ultrasound machine into a cutting-edge, hospital-wide POCUS program